Eating Disorders
Disclaimer
These guidelines have been produced to guide clinical decision making for general practitioners (GPs). They are not strict protocols. Clinical common-sense should be applied at all times. These clinical guidelines should never be relied on as a substitute for proper assessment with respect to the particular circumstances of each case and the needs of each patient. Clinicians should also consider the local skill level available and their local area policies before following any guideline.
|
|
If a patient is experiencing severe physiological or psychiatric instability with imminent risk to self or others, please refer to the nearest Emergency Department
|
Introduction
Many psychological disorders and physical illnesses experienced by children and adolescents (young people) involve disordered eating. One third of all adolescents have experienced dissatisfaction with their body weight or had unhealthy weight control practices1.Up to 41% of adolescent females experienced disordered eating1.
Eating disorders are highly complex, serious mental illnesses with significant physical complications and psychosocial impairment. The early identification and treatment of an eating disorder is essential for a positive prognosis. Treatment should be provided in a stepped-care approach, with young people and their families stepping up to more intensive care, or back down to less intensive care, as indicated5.
Services for children and adolescents presenting with eating disorders are delivered across multiple settings, including Community Child and Adolescent Mental Health Service (CAMHS), Perth Children’s Hospital Emergency Department (PCH ED), PCH Adolescent Medicine (Ward 4A) and the CAMHS Eating Disorder Service (EDS).
The CAMHS EDS is a Tier 4 state-wide specialist service, offering assessment to young people up to 16 years of age with severe eating disorders including:
- Anorexia Nervosa
- Bulimia Nervosa
- Atypical Anorexia Nervosa
- Binge Eating Disorder
- Avoidant Restrictive Food Intake Disorder (ARFID - if high school-aged)
- Eating Disorders Not Otherwise Specified (EDNOS)
To ensure a patient is accepted into this service, please demonstrate that Tier 1-3 services have been insufficient, or are unlikely to succeed. The outcome of an assessment may be to offer treatment with EDS, and if indicated can continue to be accessed up to 18 years of age.
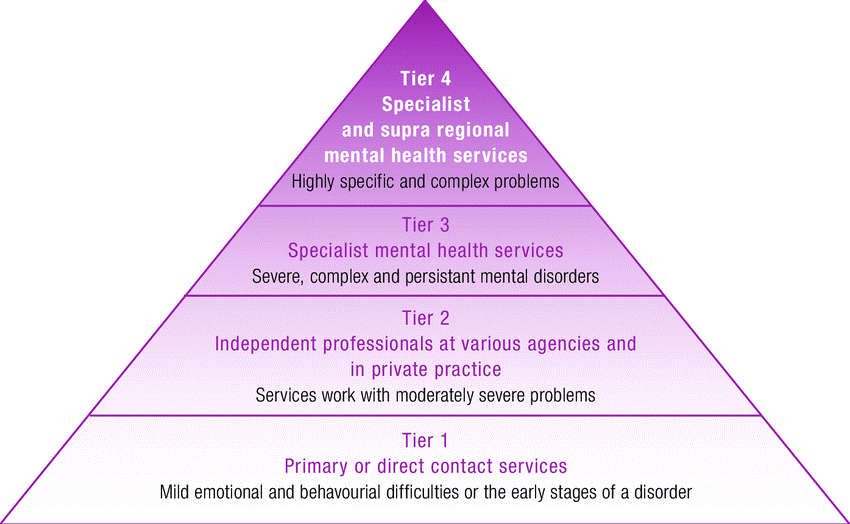
Figure 1: The mental health tiered system of care
Pre-referral investigations
- Thorough history taking including:
- Seemingly unrelated psychological and physical complaints e.g. stress, depression, anxiety, menstrual irregularities, dizziness
- Exploration of body dysmorphia/over-evaluation of weight/shape
- Evidence of weight controlling behaviours (restriction, exercise, purging) including duration, frequency, severity
- Gastrointestinal symptoms including abdominal pain, nausea, vomiting, constipation & food intolerance
- General Medical Examination including:
- Cardiovascular
- Respiratory
- Abdominal
- Neurological
- Dermatological
- Assessment of physiological compromise (see Figure 2 for admission indicators):
- Postural instability: pulse & BP on lying and standing after 1 minute
- Temperature
- Weight, Height and BMI
- FBC
- U&E
- LFT
- BGL (random)
- Urinalysis
- Iron studies
- IGF1
- B12, folate, Vitamin D
- Calcium, Magnesium, Phosphate
- Hormonal testing-TFT, FSH, LH, oestradiol, prolactin
- ECG including measurement of corrected QTc interval
- Results of any recent imaging studies
See ‘Physical Health Form’ in the Useful Resources Section below as a guide when reviewing a patient
| Risk |
High concern |
Significant concern |
Moderate concern |
| % median BMI |
<70% |
>70 – 80% |
>80 – 90% |
Recent weight loss over
3 consecutive weeks |
>1kg / week |
0.5 – 1kg / week |
<0.5kg / week |
| Awake heart rate (HR) |
<45 beats / min |
<50 beats / min |
50–60 beats / min |
| Postural change |
>50 |
>30 |
|
| Rhythm |
Any arrhythmia
ST or T-wave change |
|
|
| Syncope |
Recurrent |
Occasional |
Pre syncope |
| Blood pressure (BP) |
<80 / 40 |
< 90 / 50 |
|
| Postural systolic BP fall |
20mmHg |
15mmHg |
<15mmHG |
| QTc ms |
>450 |
|
|
| Oedema |
Present |
|
|
| Tympanic temperature |
<35.5°C |
|
|
| Extremities |
Cold / blue /
pressure sores present |
|
|
| Dehydration |
Moderate – severe |
Mild |
|
| Biochemical |
Significant electrolyte disturbance
Hypoalbuminaemia
Hypoglycaemia <3.0 mmol/L
Hypokalaemia <3.0 mmol/L
Hypophospataemia <0.9 mmol/L
|
|
|
|
DISORDERED EATING BEHAVIOUR |
| Acute food refusal |
3 days |
<50% of required |
50% of required |
| Purging / vomiting |
After all intake |
Multiple times per day |
|
Behaviour relating to
meal support and limits
|
Violent |
Unable to implement meal plan |
|
| Activity / exercise |
Uncontained
>2hrs/day |
Moderate
>1hr/day |
Mild
<1hr/day |
| |
SIGNIFICANT MENTAL HEALTH CONCERNS |
| Self-harm |
Overdose |
Active self-harm |
|
| Suicidality |
Moderate to high |
Low level suicidal ideation |
|
Figure 2: Indicators for admission. Criteria adapted from the RANZCP (2014) and NSW (2014) Guidelines4, 5
Pre-referral management
Please see the management and referral pathways for patients outlined in these documents:
Other useful resources for management:
When to refer
<16 years of age with significant physiological instability:
- Promptly contact the PCH Adolescent Medical On-Call Consultant Paediatrician via PCH Switchboard to formulate a plan regarding need for assessment and/or admission
Significant psychiatric instability with non-imminent concerns about risk:
16-18 years of age with significant physiological instability:
How to refer
Essential information to include in your referral
- Name and details of patient and caregiver, including hospital (UMRN) number and Medicare number if known
- Current therapeutic engagement: provider/s and duration
- Current medication (including any allergies)
- Results of any investigations
- Clear documented evidence of:
- significant weight concerns (or restrictive diet if ARFID) and,
- significant physical sequelae of weight loss, and
- of body image distortions (or restrictive diet if ARFID)
- maximum weight with dates & minimum weight with dates (to enable estimation of rate of change)
- Demonstrate that Tiers 1-3 have been insufficient or why they are unlikely to succeed due to the complexity of the patient’s situation, or the family’s inability to access Tier 2-3 services (e.g. for financial reasons)
Useful resources
References
- Sparti, C., Santomauro, D., Cruwys, T., Burgess, P., Harris, M. (2019). Disordered eating among Australian adolescents: Prevalence, functioning, and help received. International Journal of Eating Disorders, 52: 246254, doi: 10.1002/eat.23032 https://pubmed.ncbi.nlm.nih.gov/30734332/
- Telethon (2015) Second Australian Child and Adolescent Survey of Mental Health and Wellbeing
https://www.health.gov.au/resources/publications/the-mental-health-of-children-and-adolescents
- Hay P, Current approach to eating disorders: a clinical update, Internal Medicine Journal 50 (2020) 24–29
- Van Eaden, A et al, Incidence, prevalence and mortality of anorexia nervosa and bulimia nervosa, Curr Opin Psychiatry (2021) 34:515–524
- National Eating Disorders Collaboration Developing Practical Approaches to Eating Disorders, 2013
| Reviewer/Team: |
Adolescent Medicine & Child and Adolescent Mental Health Service-Eating Disorders
|
Last reviewed: |
Nov 2022 |
|
|
Review date: |
Nov 2025 |
This document can be made available in alternative formats on request for a person with a disability.