Hypercyanotic spells
Disclaimer
These guidelines have been produced to guide clinical decision making for the medical, nursing and allied health staff of Perth Children’s Hospital. They are not strict protocols, and they do not replace the judgement of a senior clinician. Clinical common-sense should be applied at all times. These clinical guidelines should never be relied on as a substitute for proper assessment with respect to the particular circumstances of each case and the needs of each patient. Clinicians should also consider the local skill level available and their local area policies before following any guideline.
Read the full PCH Emergency Department disclaimer.
|
Aim
To guide staff with the assessment and management of hypercyanotic spells in children.
Background
- Infants with unrepaired tetralogy of Fallot or other congenital cardiac defects causing dynamic right ventricular outflow tract obstruction (RVOTO) are at risk of hypercyanotic spells (also referred to as tet spells).
- Hypercyanotic spells may occur at any stage of life but are more common at 2 – 6 months of age.
- The spell is caused by an acute reduction in pulmonary blood flow associated with an increase in the magnitude of the right-to-left shunt.
- Hypercyanotic spells are characterised by:
- Period of uncontrollable crying / irritability
- Hyperpnoea (rapid, deep respiration)
- Worsening hypoxia with cyanosis/pallor
- Decreased intensity of heart murmur
- Limpness, loss of consciousness or convulsions
- Death (in severe or untreated episodes)
- Common precipitants include stressful situations, extreme crying, straining during defaecation, feeding, waking from a nap, fever and dehydration.
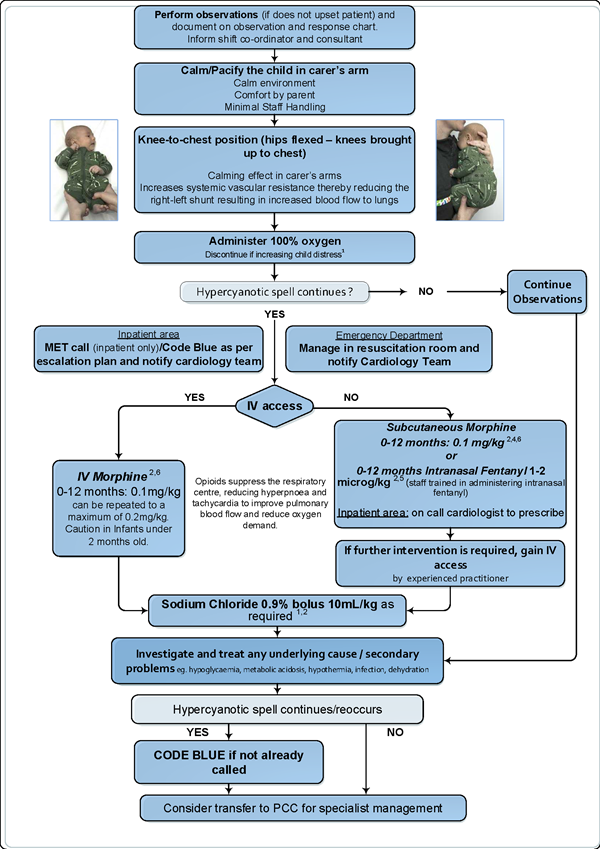
Management
Treatment of spells involves the following management steps in order of increasing complexity:
Bibliography
- J Grossett, A Kamp. Tetralogy of Fallot. Management of hypercyanotic spells. London: British Medical Journal. Best Practice. 2020 [updated March10th 2020]. https://bestpractice.bmj.com/topics/en-gb/701
- Doyle,T, Kavanaugh-McHugh, A, Fish,F. Management and outcome of tetralogy of Fallot. Oct 30 2019. https://www.uptodate.com/contents/management-and-outcome-of-tetralogy-of-fallot
- Morphine: Drug information. Dosing: Pediatric. Lexicomp. UpToDate [Accessed September 2021]. Available from: https://www-uptodate-com.pklibresources.health.wa.gov.au/contents/morphine-drug-information?search=tet%20spell&topicRef=5770&source=see_link#F8776810
- Tsze DS, Vitberg YM, Berezow J, Starc TJ, Dayan PS. Treatment of Tetralogy of Fallot Hypoxic Spell With Intranasal Fentanyl. Pediatrics.2014. 134 (1)
- PCH Emergency Department. Dr Dennis Chow. Fentanyl in Hypercyanotic spells. (Expert Opinion) 2021
- PCH Cardiology Department. Dr Stephen Shipton. Morphine in Hypercyanotic spells (Expert opinion) 2021
- Starship Children’s Hospital. Tetralogy of Fallot (Clinical Guideline) Auckland, NZ 2010 [Accessed February 2021]. Available from: https://www.starship.org.nz/for-health-professionals/starship-clinical-guidelines/t/tetralogy-of-fallot
- Royal Children’s Hospital Melbourne. Cyanotic Episodes (Spells) Clinical Practice Guidelines [Internet]. 2005 2 May 2014. Available from: https://www.rch.org.au/clinicalguide/guideline_index/Cyanotic_episodes_spells/
| Endorsed by: |
Drugs and Therapeutics Committee |
Date: |
Oct 2021 |
This document can be made available in alternative formats on request for a person with a disability.