Gastroenteritis
Disclaimer
These guidelines have been produced to guide clinical decision making for the medical, nursing and allied health staff of Perth Children’s Hospital. They are not strict protocols, and they do not replace the judgement of a senior clinician. Clinical common-sense should be applied at all times. These clinical guidelines should never be relied on as a substitute for proper assessment with respect to the particular circumstances of each case and the needs of each patient. Clinicians should also consider the local skill level available and their local area policies before following any guideline.
Read the full CAHS Emergency Department disclaimer.
|
Aim
To guide Emergency Department (ED) staff with the assessment and management of gastroenteritis.
Background1,2,3
Gastroenteritis is vomiting, diarrhoea or both caused by viruses in 70% of cases, bacteria in 20% and protozoa in 10% of cases.
- Vomiting may occur before the onset of diarrhoea. However, vomiting in isolation may be due to a wide range of other potentially serious conditions.
- Concerning features suggesting an alternate diagnosis are significant abdominal pain, co-morbidities, < 6 months age, high fever, prolonged symptoms, or signs suggesting a surgical cause.
- In infants, vomiting must be distinguished from the normal phenomenon of regurgitation.
- Oral / nasogastric tube (NGT) / orogastric tube (OGT) rehydration is preferable to intravenous except in severe cases.
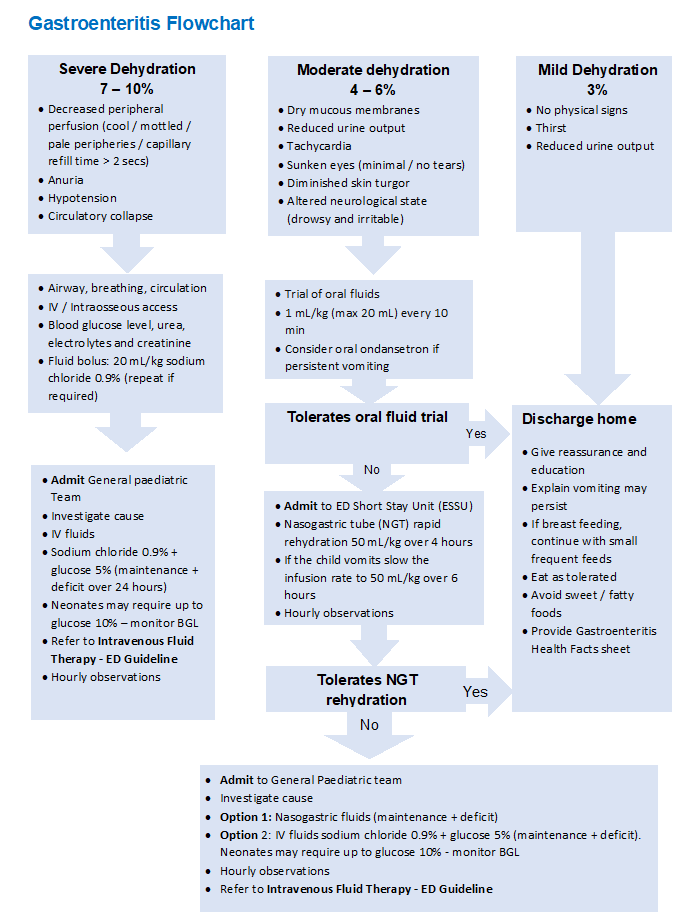
Gastroenteritis flowchart
Risk factors for developing gastroenteritis
- Attending childcare
- Recent travel overseas
Assessment2,3
- Evaluation of the severity of dehydration is difficult even by a senior doctor.
Examination
| No or mild dehydration |
<3% weight loss |
No physical signs, + / - thirst, dry mucus membranes, reduced urine output |
| Moderate dehydration |
4-6% weight loss |
Dry mucus membranes, reduced urine output, tachycardia, sunken eyes, minimal or no tears, diminished skin turgor, altered neurological status (drowsiness and irritability). |
| Severe dehydration |
7-10% weight loss |
Increasingly marked signs from the above group, plus: decreased peripheral perfusion, (cool, mottled, pale peripheries, capillary refill time >2 seconds), anuria, hypotension, circulatory collapse. |
Investigations
- No investigations are required in mild cases of gastroenteritis
- Stool specimen is required for patients with bloody stool, prolonged diarrhoea and recent travel overseas
- Full blood count (FBC), urea, electrolytes and creatinine (UEC), blood glucose level (BGL) and venous blood gas (VBG) should be done if inserting an intravenous cannula to commence intravenous fluids
Differential diagnoses1,2
- Urinary tract infection
- Appendicitis
- Meningitis
- Diabetic ketoacidosis (DKA)
- Haemolytic uraemic syndrome
- Congenital adrenal hyperplasia
- Irritable bowel disease
- Intussusception
Management1,3,4
- Non dehydrated children can be discharged after reassurance, education and a health fact sheet to go home. A trial of fluid is not required in ED.
- Non dehydrated children can eat as tolerated but should avoid sweet and fatty foods.
- Continue breastfeeding – extra fluids can be added as required.
- Ondansetron may be used in the ED before a fluid trial but not as a discharge medication. It can make the diarrhoea last longer.5
- In moderately dehydrated children oral / nasogastric rehydration is preferable to intravenous as it corrects acidosis quicker, the diarrhoea and vomiting settle faster and appetite returns sooner.
- Severe dehydration needs admission for intravenous rehydration and electrolytes need to be checked.
Further management
| Mild dehydration |
- Oral fluids: 1 mL/kg every 10 minutes of oral rehydration solution or water (if dislikes ORS) or watered down apple juice can be provided whist awaiting medical assessment.
- Fluids high in sugar (cola, apple juice, sports drinks, containing ≤ 20 mmol/L sodium with osmolality 350-750 mOsm/L) should be avoided.
- Solids and milk can be continued if the child is interested and not dehydrated.
- Most mildly dehydrated children can be discharged.
- On discharge: ensure the caregiver is discharged with appropriate education on gastroenteritis, including how to provide fluid and signs of dehydration.
|
| Moderate dehydration |
- Oral fluid trial of 1 mL/kg every 10 minutes of oral rehydration solution for 1-2 hours.
- Fluids high in sugar (cola, apple juice, sports drinks, containing ≤ 20 mmol/L sodium with osmolality 350-750 mOsm/L) should be avoided.
- Solids and milk can be continued if the child is interested and not dehydrated otherwise wait until rehydrated.
- Consider oral ondansetron4,5 if persistent vomiting to facilitate oral fluid intake:
- > 6 months and 8–15 kg, oral 2 mg as a single dose.
- 15–30 kg, oral 4 mg as a single dose.
- > 30 kg, oral 8 mg as a single dose.1
|
| Severe dehydration |
- Insert IV cannula, check FBC, UEC and VBG.
- IV fluid bolus: 20 mL/kg bolus of sodium chloride 0.9% (repeat if required) and admit under the General Paediatric team.
- Investigate possible underlying causes.
- Continue IV fluids: sodium chloride 0.9% + glucose 5% (maintenance + deficit over 24 hours). Neonates may require IV fluid with glucose 10%. BGL should be monitored in all neonates on IV fluid therapy.
If hypernatraemia (sodium >150 mmol/L) IV fluids are to be given over 48-72 hours.
|
If the child fails oral fluid trial:
- Nasogastric tube (NGT) rapid rehydration: 50 mL/kg over 4 hours with oral rehydration solution (ORS). This corrects for 5% dehydration.
- Admit to the Emergency Department Short Stay Unit (ESSU)
- If the child vomits reduce the rapid rehydration rate to 50 mL/kg over 6 hours.
If the child fails NGT rapid rehydration (> 2 vomits):
- Admit to General Paediatric team.
- Option 1: NGT fluid (maintenance + deficit).
- Option 2: IV fluids sodium chloride 0.9% + glucose 5% (maintenance + deficit).
Use the following paediatric fluid rate calculator:
|
1. Deficit volume
- Deficit volume = weight (kg) x % dehydration x 10 mL
|
|
2. Maintenance
<10 kg = 100 mL/ kg / 24 hours
10-20 kg = 1000 mL + (50 mL for each kg over 10 kg) / 24 hours
>20 kg = 1500 mL + (2 0mL for each kg over 20 kg) / 24 hours
|
|
3. Hourly rate
- Hourly rate = (deficit volume + 24 hours maintenance fluids) divided by 24
|
Medication
- Ondansetron can be used before a fluid trial or if the child vomits during rapid rehydration. It is not recommended as a discharge medication.
- No other anti-emetics or anti-diarrhoeal agents are to be used in infants or children with suspected gastroenteritis.
Admission criteria
- Failed rapid rehydration with OGT or NGT
- Severe dehydration requiring intravenous fluids.
Referrals and follow-up
- Patients with mild to moderate dehydration who are sent home after oral fluid trial should have a GP review at 24 hours.
Nursing
- Ensure all children are weighed on admission for assessment of dehydration and to provide a base weight (bare weight < 12 months old, light clothing for all other children)
- Ensure the child is reweighed prior to discharge
- Utilise the appropriate rehydration form if the child is having a trial of fluids
Observations
- Complete and record a full set of observations on the Observation and Response Tool and record additional information on the Clinical Comments chart.
- Complete a full set of neurological observations if clinically indicated.
- Minimum of hourly observations at least.
- Fluid input / output is to be monitored and documented.
- BGL and ketones (if frequent vomiting and not tolerating fluids).
References
- Guarino A, Ashkenazi S, Gendrel D, Lo Vecchio A, Shamir R, Szajewska H. European Society for Pediatric Gastroenterology, Hepatology, and Nutrition/European Society for Pediatric Infectious Diseases evidence-based guidelines for the management of acute gastroenteritis in children in Europe: update 2014. J Pediatr Gastroenterol Nutr. 2014;59(1):132
- O’Ryan MG, UpToDate:Acute viral gastroenteritis in children in resource-rich countries: Clinical features and diagnosis. 2022 UpToDate
- National Institute for Health and Care Excellence. Diarrhoea and vomiting in children: Diarrhoea and vomiting caused by gastroenteritis: diagnosis, assessment and management in children younger than 5 years. https://www-nice-org-uk.pklibresources.health.wa.gov.au/guidance/cg84
- O’Ryan MG, UpToDate: Acute viral gastroenteritis in children in resource-rich countries: Management and prevention. 2022. UpToDate
- AMH Children’s Dosing Companion (2021) Australian Medicines Handbook Pty Ltd 2021, [Internet] Ondansetron; [Modified July 2021, Cited 18 Oct 2021,] Available from: Ondansetron
- IBM Micromedex IBM Corporation Ondansetron Hydrochloride. Last Updated 12 January 2022. Cited 15 March 2022. Available from: Drug Result Page - Quick Answers - Dosing/Administration - Pediatric Dosing (health.wa.gov.au)
| Endorsed by: |
CAHS Drug & Therapeutics Committee |
Date: |
June 2023 |
This document can be made available in alternative formats on request for a person with a disability.