Cervical spine trauma
Disclaimer
These guidelines have been produced to guide clinical decision making for the medical, nursing and allied health staff of Perth Children’s Hospital. They are not strict protocols, and they do not replace the judgement of a senior clinician. Clinical common-sense should be applied at all times. These clinical guidelines should never be relied on as a substitute for proper assessment with respect to the particular circumstances of each case and the needs of each patient. Clinicians should also consider the local skill level available and their local area policies before following any guideline.
Read the full CAHS clinical disclaimer
|
Aim
To guide staff with the assessment and management of cervical spine trauma.
Key points
- Cervical spine injury should be suspected in all children with serious trauma, in particular in those with severe head injury.
- Australian and New Zealand Committee on Resuscitation (ANZCOR), International Liaison Committee on Resuscitation (ILCOR) and the State Spinal Cord Injury Service no longer recommend rigid cervical collar use in initial cervical spine immobilisation.
- Senior clinicians must assist in the assessment of children with suspected cervical spine injury to facilitate early removal of cervical spine immobilisation where appropriate and to limit exposure to radiation with imaging.
- The majority of paediatric trauma patients will not require neck imaging.
Background
- Suspected neck injuries are a common presentation to the emergency department, however, significant cervical spine injury following blunt trauma is uncommon occurring in only approximately 1% of all paediatric blunt trauma2.
- Children <8 years are more prone to sustaining high injuries (C1-C3) due to anatomical differences when compared to older children.
- Children >8 years have similar injury patterns to those seen in adults2.
Cervical spine assessment and identification of cervical spine injury is difficult. There is currently no validated clinical decision rule for use in paediatrics. The Canadian C-spine Rule and National Emergency X-Radiography Low Risk Criteria (NEXUS) can be used to determine the need for imaging in adults; however, these are not currently validated in paediatrics.
The Paediatric Emergency Care Applied Research Network (PECARN) has identified the following risk factors for cervical spine injury in children who have sustained blunt trauma (with an associated 98% sensitivity)3:
- Altered mental status (Glasgow Coma Score (GCS) <15)
- Focal neurological deficits
- Complaint of neck pain
- Torticollis
- Substantial injury to the torso
- Predisposing condition
- Diving injury
- High-risk motor vehicle accident (MVA) (head-on collision, rollover, ejected from the vehicle, death in the same accident, high speed >88km/hr).
Assessment3
History
- High risk mechanism of injury:
- High risk MVA as above
- Axial load to the head (trampoline, diving, fall from height)
- Substantial torso injury
- Persisting symptoms of neck pain, paraesthesia or weakness
- Predisposing factors for cervical spine injury such as trisomy 21, osteogenesis imperfecta, achondroplasia, other rheumatological, genetic or metabolic conditions or previous spinal surgery.
Examination
Pre-requisites for reliable examination:
- Alert (GCS ≥14)
- Not affected by drugs / alcohol / sedative analgesia
- Adequately cooperate with examination (can have other significant injuries if they can focus throughout entire examination)
Examining the cervical spine:
- Provide analgesia and minimise neck movements
- Palpate for tenderness along spinous processes from nuchal ridge to first thoracic vertebrae
- Palpate lateral to the midline on right and left sides
- Assess for sensory and motor neurological deficit
- If no significant tenderness and no abnormal neurology, assess active range of lateral rotation to 90 degrees and range of flexion and extension (chin to chest and look up) – stop if develops significant pain or neurological deficit
Red flags:
- Traumatic torticollis
- Objective and persisting neurological deficit
- Child using hands to hold head or neck
- Restrictive neck movement
- Refractory hypotension (consider spinal shock)
Investigations
Clinical C-spine Clearance
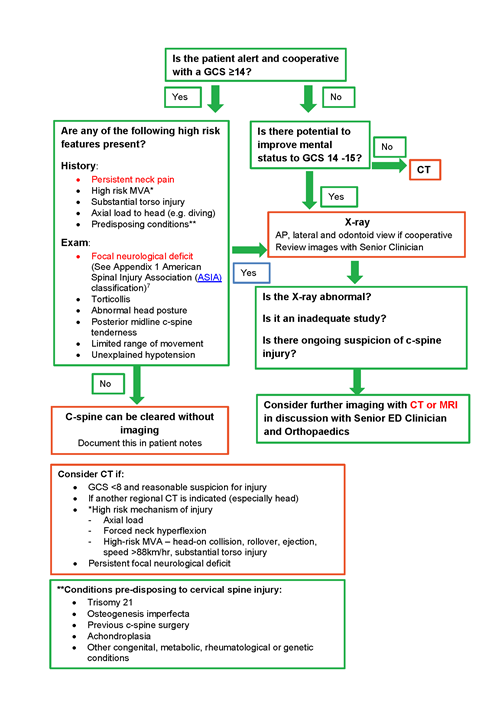
Download the C-Spine clearance tool (PDF).
CT scan +/- MRI (with urgent Orthopaedic review) should be the initial imaging of choice in patients with abnormal neurological findings and all unconscious patients.
Plain radiology has the advantage of a lower dose of radiation but has reduced sensitivity (<90%). It should be the initial assessment tool of choice in cases assessed as relatively lower risk4.
Management
- Immobilisation and spinal precautions should be maintained for all children with suspected cervical spine injury.
- Priority of treatment should be given to life-threatening airway, breathing or circulatory problems, along with early attention to spinal immobilisation.
- If <8 years old, consider torso elevation with an aeroplane pillow to maintain neutral spine alignment6. These can be found on ward 1B.
- There is little evidence to support spinal immobilisation devices such as hard cervical collars. They are not without complications and significant attempts to restrict spontaneous movement in an uncooperative child should be avoided.
- If patient is in a hard collar, change to a soft collar (Philadelphia, Miami J or similar) early to avoid prolonged periods in a hard collar and potential for pressure injury.
- Head blocks or towel bollards can be used as a reminder for the patient to limit head movement.
Application of Miami J Collar
Refer to Miami J Collar - ED Guideline for further information regarding sizing and application.
Moments of Risk
- Log rolls and bed transfers
- Perform manual in-line stabilisation for all transfers and log rolls
- Consider use of a patient slide board for transfers
- The transfer / logroll will be coordinated by the staff member in control of the patient’s head
- Vomiting
- Consider antiemetics early or nasogastric if appropriate
- Log roll if vomiting
- Intubation
- Specific staff member assigned to perform manual in-line stabilisation
- Prepare for difficult airway
- Pain / agitation
- Early analgesia
- Reassurance by staff and family member – keep at head end of bed if possible
- In conscious infants, allow to find position of comfort
Nursing
- Undertake regular pressure area care whilst in ED.
Patient Transfers
When transferring a patient from the ED trolley to the ward bed:
- Receiving ward staff will assume control of the patient’s head prior to the transfer/logroll
- The transfer/logroll will be coordinated by the staff member in control of the patient’s head
- ED staff will assist with the transfer/logroll as required.
Observations
- Complete and record a full set of observations on the observation and response tool and record additional information on the Clinical Comments chart
- Complete a full set of neurological observations if clinically indicated
- Minimum hourly observations whilst in ED.
References
- Kwan, I., Bunn, F. & Roberts, I. 2009. Spinal immobilisation for trauma patients. Cochrane Database of Systematic Reviews (Online).
- Mohseni, S., Talving, P., Branco, B. C., Chan, l. S., Lustenberger, T., Inaba, K., Bass, M. & Demetriades, D. 2011. Effect of age on cervical spine injury in pediatric population: A National Trauma Data Bank review. Journal of Pediatric Surgery, 46, 1771- 1776
- Leonard, Julie C et al. “Factors associated with cervical spine injury in children after blunt trauma.” Annals of emergency medicine vol. 58,2 (2011): 145-55.
- Hopper, Sandy M, Stewart McKenna, Amanda Williams, Natalie Phillips, and Franz E Babl. "Clinical Clearance and Imaging for Possible Cervical Spine Injury in Children in the Emergency Department: A Retrospective Cohort Study." Emergency Medicine Australasia 32.1 (2020): 93-99. Web.
- Herman M 2019, Paediatric Cervical Spine Clearance. A Consensus statement and algorithm from the Paediatric Cervical Spine Clearance Working Group, The Journal of Bone and Joint Surgery, 101:1:1-9
- Pandie Z, S. M., Lamont T, Walsh M, Phillips M, Page C 2009. Achieving a neutral cervical spine position in suspected spinal cord injury in children: analysing the use of a thoracic elevation device for imaging the cervical spine in paediatric patients. Emerg Med J, 2010, 573-576
- Roberts, T. T., Leonard, G. R., & Cepela, D. J. (2017). Classifications In Brief: American Spinal Injury Association (ASIA) Impairment Scale. Clinical orthopaedics and related research, 475(5), 1499–1504. Classifications In Brief: American Spinal Injury Association (ASIA) Impairment Scale (nih.gov)
| Endorsed by: |
Nurse Co-director, Surgical Services |
Date: |
Apr 2022 |
This document can be made available in alternative formats on request for a person with a disability.