Inhaled foreign body
Disclaimer
These guidelines have been produced to guide clinical decision making for the medical, nursing and allied health staff of Perth Children’s Hospital. They are not strict protocols, and they do not replace the judgement of a senior clinician. Clinical common-sense should be applied at all times. These clinical guidelines should never be relied on as a substitute for proper assessment with respect to the particular circumstances of each case and the needs of each patient. Clinicians should also consider the local skill level available and their local area policies before following any guideline.
Read the full CAHS clinical disclaimer
|
Aim
To guide Emergency Department (ED) staff with the assessment and management of inhaled foreign bodies.
Assessment1,2
History
- Sudden respiratory arrest and collapse can be caused by complete obstruction of the upper airway by an inhaled foreign body (FB)
- There may be a history of choking, gagging or coughing during eating or playing, and sometimes carers see the child with something in their mouth before the event
- Occasionally, children who were not previously suspected to have inhaled a foreign body may present to ED with persistent cough or wheezing
- Pneumonia not responding to treatment or recurrent pneumonia in the same lobe / segment should raise concerns about an inhaled foreign body
Examination2
- Stridor indicates a partial obstruction of the upper airway by an inhaled foreign body
- Clinically there may be asymmetric chest movement and / or asymmetric breath sounds
- A foreign body acting as a ball valve may cause air trapping with subsequent hyperinflation of the particular lung / lobe and deviation of the trachea
- There may be localised wheezing, crackles or decreased breath sounds, or signs of consolidation suggesting collapse of a lobe / segment
- In some children there will be no abnormal findings
Investigation2,3
- Radiological studies are only indicated if there is doubt regarding the presence of a foreign body
- Children with history and examination findings suggestive of inhaled foreign body should be referred to the respiratory specialist
If history and / or examination findings are inconclusive, imaging should be performed as follows:
- In hours: CT chest (request to state ‘?bronchial foreign body’). This is based on sensitivity and specificity approaching 100% with a radiation dose similar to conventional chest X-ray
- After hours: Inspiratory and expiratory Posterior / Anterior (PA) chest X-rays, plus a lateral chest X-ray looking for:
- An opaque foreign body may occasionally be seen. The lateral chest X-ray will confirm its presence in the bronchial tree as opposed to the oesophagus.
- Segmental or lobar collapse
- Difference in lung expansion between the two sides
- Localised hyperinflation or interstitial emphysema may result from a ball valve obstruction
- Be aware that chest X-ray may be normal and if a FB is strongly suspected the child should be discussed with the respiratory team for follow up
Management
For suspected upper airway foreign bodies1
- Allow the child to sit upright in the position in which they are most comfortable
- If airway is compromised refer to Choking – PCH ED Guideline
- Urgent referral to ENT and respiratory team referrals
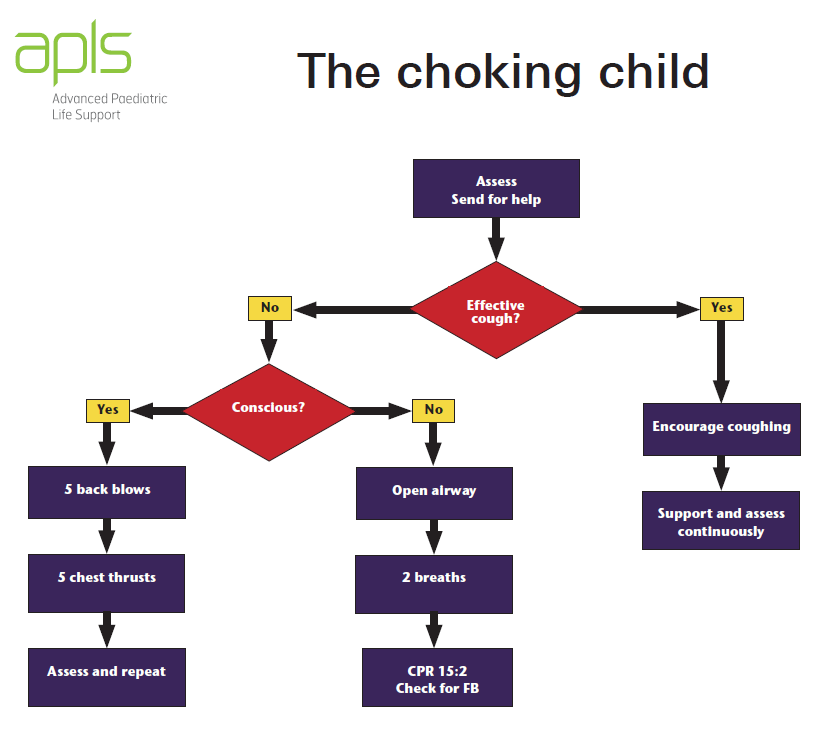
*APLS – Algorithms - The Choking Child4
Indications for referral to respiratory medicine for suspected lower airway foreign bodies
- Cases which meet 2 out of 3 of the following criteria:
- Suggestive history and / or symptoms that could be explained by inhaled FB
- Examination findings compatible with an inhaled FB
- Radiological changes compatible with an inhaled FB
- The respiratory team will contact ENT if a bronchoscopy is indicated
- Fast from time of clinical suspicion
References
- Martin Samuels, Sue Wieteska. Advanced Paediatric Life Support: A Practical Approach to Emergencies, Sixth Edition. Wiley Blackwell. 2017
- Ruiz F, 2022, Airway foreign bodies in children, UpToDate [Last updated: June 2022. Cited: 29 March 2023.] Available from: Airway foreign bodies in children - UpToDate (health.wa.gov.au)
- Reid A et al. Ten years of paediatric airway foreign bodies in Western Australia. Int J Paed Otorhinolaryngology 2020 Feb;129:109760
- Choking child algorithm. Advanced Paediatric Life Support 2020. [Cited 11 May 2022] Available from: Algorithms | The choking child (apls.org.au)
| Endorsed by: |
Nurse Co-Director, Surgical Services |
Date: |
Apr 2023 |
This document can be made available in alternative formats on request for a person with a disability.