Meningococcal disease
Disclaimer
These guidelines have been produced to guide clinical decision making for the medical, nursing and allied health staff of Perth Children’s Hospital. They are not strict protocols, and they do not replace the judgement of a senior clinician. Clinical common-sense should be applied at all times. These clinical guidelines should never be relied on as a substitute for proper assessment with respect to the particular circumstances of each case and the needs of each patient. Clinicians should also consider the local skill level available and their local area policies before following any guideline.
Read the full CAHS clinical disclaimer
|
Meningococcal disease can have significant overlap with sepsis and meningitis.
There are separate guidelines available for these conditions:
Separate guidelines also exist for the care of neonates:
Aim
To guide PCH Emergency Department (ED) staff with the assessment and management of meningococcal disease.
Background1,2
- Invasive meningococcal disease is a rapidly fatal disease if not recognised and treated.
- The mortality rate is 10% despite appropriate antibiotic therapy.
- Failure to quickly recognise and treat this disease can result in increased morbidity and mortality.
Key points1,2
- Asymptomatic nasopharyngeal carriage of meningococci is common.
- Approximately 10% of the population are carriers at any one time.
- Invasive infection with Neisseria meningitides (meningococcus) occurs in endemic and epidemic forms.
- Meningococcus presents as bacterial meningitis (15% of cases) or septicaemia (25% of cases), or as a combination of the two presentations (60% of cases).
- The overall mortality risk is high (about 10%) despite appropriate antibiotic therapy.
- Meningococcal septicaemia (also known as meningococcaemia) has considerably greater mortality than meningococcal meningitis and is often characterised by a rapidly evolving petechial or purpuric rash that does not blanch under pressure.
- Meningococcaemia can have a fulminant and rapidly fatal course.
- Early administration of antibiotics on suspicion of meningococcal disease can be lifesaving.
- The disease is transmitted via respiratory droplets, and has an incubation period of between 1 and 10 days, but commonly 3 to 4 days.
Assessment2
- A non-blanching purpuric or petechial rash is typical but may not be present, particularly in early disease.
- Recognise signs of shock and treat aggressively after antibiotic therapy - see Sepsis recognition and management.
History
- The early symptoms of meningococcal disease may mimic those associated with common viral infections. However, once the infection is established symptoms can progress rapidly, with death sometimes occurring only hours from the onset of symptoms.
- Influenza virus or Mycoplasma pneumoniae infections may predispose to invasive disease.
Meningococcal Meningitis
- Characteristically has sudden onset and rapidly progressive symptoms.
- The classical meningitis triad of fever, stiff neck and headache is not always present. Myalgia and altered mental status is often present.
- An associated late sign is a petechial rash, but this is not always present
- Infants will not develop signs of meningism. The most common symptoms and signs for infants include fever, tachypnoea, rash, vomiting, poor feeding, irritability, drowsiness, and pallor.
Meningococcal Septicaemia
- Usually presents with an acute febrile illness, shock, profound malaise, myalgia or arthralgia, nausea and vomiting, altered consciousness, and a maculopapular / petechial rash (50% of cases).
- The most characteristic feature is a haemorrhagic (i.e. petechial or purpuric) rash that does not blanch under pressure. However, the rash may begin as non-specific, be similar to a viral exanthem, or not be present at all. The rash can appear on any part of the body, including the palms and soles, and progress rapidly.
- A rash is not always present, especially in the early stages.
- In the early stage of development the rash may blanch with pressure thus resembling a viral exanthema.
- The rash can appear on any part of the body, including the palms and soles, and progress rapidly.
- The petechial rash has discrete 1-2 mm lesions which may evolve to form larger ecchymosis. They commonly appear in clusters in areas where pressure occurs (e.g. underwear elastic bands), and children being examined should always be completely undressed.
- Meningococcal septicaemia is more often misdiagnosed than meningococcal meningitis at first presentation and has a higher fatality rate - see Sepsis recognition and management.
Meningococcal Conjunctivitis
- Rarely, meningococcal disease can present as conjunctivitis.
- This can lead to invasive disease and requires systemic therapy.
Investigations
- Treatment with antibiotics should not be delayed while awaiting laboratory results.
- If possible, blood cultures should be obtained prior to antibiotic therapy
All patients should have the following investigations
Refer to PathWest Test Directory for collection requirements
| Blood culture |
Blood Culture bottle |
| Full blood count (FBC) |
EDTA tube |
| Meningococcal PCR |
EDTA tube (separate tube) |
| C-Reactive Protein |
Lithium Heparin-PST or Serum Sep. Tube-SST |
| Nasopharyngeal swab |
Charcoal swab |
| Venous Blood Gas |
Heparinised Blood Gas Syringe |
Other investigations if appropriate
| Coagulation profile: Prothrombin Time (PT) / Activated Partial Thromboplastin Time (APTT), Disseminated Intravascular Coagulation (DIC) screen |
Sodium citrate -3.2% |
| Cerebrospinal Fluid (CSF), if not contraindicated - microscopy, culture and PCR |
CSF tube 1
|
| Aspirate from skin lesion/joint - microscopy and culture |
Culture bottle, smear and/or sterile container |
Lumbar Puncture (LP)
Do not delay antibiotics for LP if a child has a spreading rash or looks unwell / septic. Antibiotics should be given prior to LP in these patients.
Contraindications for lumbar puncture in children with suspected meningitis or suspected meningococcal disease:
- Signs suggesting raised intracranial pressure: reduced or fluctuating level of consciousness, relative bradycardia and hypertension, focal neurological signs, abnormal posture or posturing, unequal, dilated or poorly responsive pupils, papilloedema, abnormal 'doll's eye' movements
- Shock
- Extensive or spreading purpura
- After convulsions until stabilised
- Coagulation abnormalities
- Platelet count below 100 x 109/litre
- Local superficial infection at the lumbar puncture site
- Respiratory insufficiency (lumbar puncture is considered to have a high risk of precipitating respiratory failure in the presence of respiratory insufficiency).
- Do not delay antibiotics for LP if a child has a spreading rash or looks unwell / septic. Antibiotics should be given prior to LP in these patients.
See Lumbar puncture.
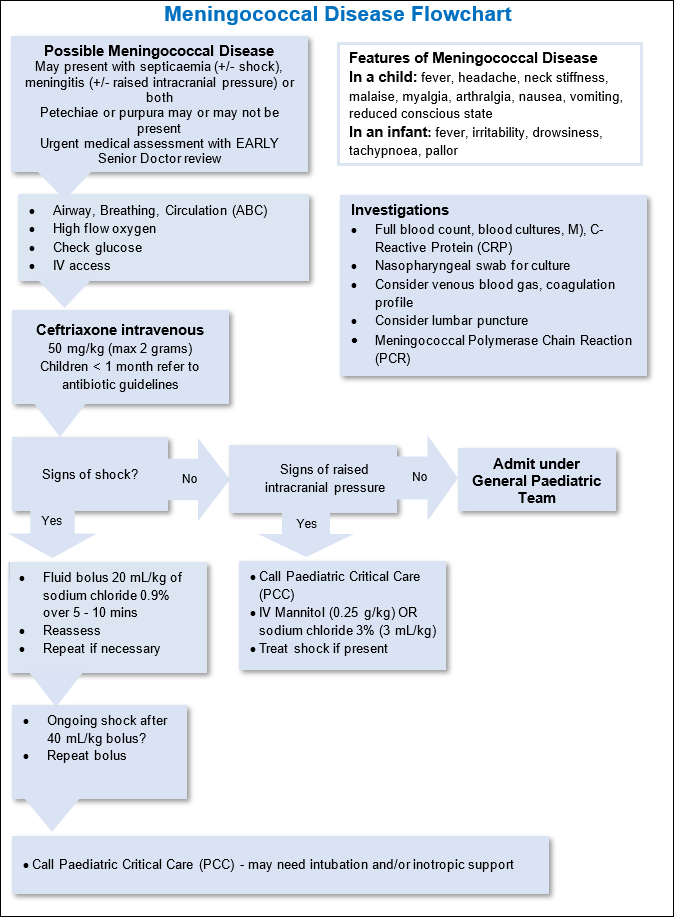
Management
- Early parenteral antibiotics will decrease mortality; do not delay antibiotic administration in suspected cases of meningococcal disease.
- Effective management of meningococcal infection requires early intervention, effective antibiotic therapy and careful attention to associated manifestations such as shock and coagulopathy.
Pre-Hospital
- It is imperative that antibiotic therapy be commenced early if deaths from meningococcal septicaemia are to be avoided.
- If a general practitioner (GP) suspects a child has invasive meningococcal disease, empiric antibiotics should be given prior to transfer to hospital.
- Ceftriaxone (preferred first option) or benzylpenicillin should be administered in doses below. The intravenous (IV) route is preferable, but intramuscular (IM) administration may be used if there is a delay in obtaining intravenous access.
- Ceftriaxone: 50 mg/kg3 (to a maximum of 2 grams) as a stat dose.
Or
- Benzylpenicillin: 60 mg/kg4 (to a maximum of 2.4 grams) as a stat dose
- If patient weight is unknown the following dose bands may be used:
Benzyl penicillin dose in suspected meningococcal disease
| Children <1 year old |
300 mg |
| Children aged 1-9 years old |
600 mg |
| Adults or children 10 years and above |
1.2 grams |
- Be aware of delayed absorption of intramuscular (IM) route if shock is present. IM route can also cause a large haematoma if disseminated intravascular coagulopathy is present. Refer to Intramuscular Injection – Clinical Practice Manual (internal WA Health only).
- Concern by the GP that the empirical use of antibiotics may obscure the diagnosis once the child reaches hospital must not prevent their early use.
- Meningococci can usually still be identified from a nasopharyngeal swab, or their DNA identified by PCR tests even if blood cultures have been sterilised by pre-hospital antibiotics.
- GPs should attempt to take blood cultures whenever possible prior to the administration of the first dose of antibiotic. The blood cultures, and any other clinical samples, should be sent with the patient at the time of transfer to hospital. However, taking of cultures should not delay initiation of treatment or transfer to hospital.
- Urgent transfer to hospital should be arranged by ambulance or Royal Flying Doctor Service (RFDS). The patient may be sick enough to require a medical escort.
Management in the emergency department
- Children referred to ED with suspected meningococcal infection or who present with symptoms and signs suggestive of meningococcal infection should be given a high priority triage category and be assessed by medical staff promptly.
Give intravenous
ceftriaxone (or
cefotaxime in neonates)
immediately to children and young people with a petechial rash if any of the following occur at any point during the assessment (these children are at high risk of having meningococcal disease):
- petechiae start to spread
- the rash becomes purpuric
- there are signs of bacterial meningitis
- there are signs of meningococcal septicaemia
- the child or young person appears ill to a healthcare professional.
Seek senior medical advice early if the patient is unwell.
- Obtain intravenous access (intraosseous if not possible).
- Take blood samples (FBC, blood culture, meningococcal PCR, CRP) and a nasopharyngeal swab.
- Administer intravenous ceftriaxone 50 mg/kg/dose (to a maximum of 2 grams) as soon as culture samples are taken. Regular ongoing doses will be required.
- Do not delay treatment
- If shocked, early and aggressive fluid therapy is critical: Give IV fluid boluses of 20 mL/kg of sodium chloride 0.9% and repeat fluid boluses until shock is corrected (BP normal and peripheral perfusion restored)
- Consider early use of vasopressors for refractory shock, in consultation with PCC
- Assess for and manage signs of cerebral oedema / raised intracranial pressure
- Consider IV steroids if suspected meningitis. Refer to Meningitis.
- Consider lumbar puncture in patients with possible meningitis. Defer LP if contraindicated (see list of contraindications above).
- The patient may require admission to PCC if they have features of septic shock, cerebral oedema, coagulopathy or vascular complications.
Medications
- Parenteral antibiotics should be administered as soon as possible in suspected meningococcal disease. Treatment for sepsis and/or meningitis should be considered as appropriate (see separate guidelines linked at the top of this guideline).
- See ChAMP Guidelines or Neonatal Monographs – Cefotaxime and Benzylpenicillin
- Discuss with PCH on call Clinical Microbiologist if any doubt.
Admission criteria
- Admit all patients with meningococcal disease under the General Paediatric Team
- A proportion of patients will require PCC admission – refer as appropriate.
Referrals and follow-up
Public Health Notification6:
- Meningococcal disease is a notifiable disease. Refer to Notification of infectious diseases and related conditions - Department of Health WA.
- Because of its public health implications, telephone notification is required for any probable meningococcal infection (do not wait for lab confirmation).
- During office hours, Monday-Friday: Call the Communicable Disease Control Directorate (metropolitan area) on 9222 0255 or the appropriate regional Public Health Unit
- After hours and weekends: Call the on-call Public Health Physician, via the Department of Health Duty Officer, on 1800 434 122.
Nursing
Isolation
- Implement Transmission Based Precautions for all patients with either suspected or confirmed meningococcal disease.
- Transmission based precautions should be applied for 24 hours after the initiation of antibiotic therapy.
- Record a full set of observations on the Observation and Response Chart as required and additional information including a description of the location and progression of any rash on the Clinical Comments Chart.
References
- Meningococcal Disease. Centres for Disease Control and Prevention. Last Updated: 7 February 2022. Cited: 9 March 2022. Available from : Meningococcal Disease Diagnosis and Treatment | CDC
- Apicella M. Clinical manifestations of meningococcal infection. [Internet] UpToDate. Last Updated: 4 October 2021. Cited 30 August 2022. Available from: Clinical manifestations of meningococcal infection - UpToDate (health.wa.gov.au)
- AMH Children’s Dosing Companion (2021) Australian Medicines Handbook Pty Ltd 2021, [Internet] Ceftriaxone; [Modified July 2021, Cited 18 Oct 2021,] Available from: Ceftriaxone - AMH Children's Dosing Companion (health.wa.gov.au)
- AMH Children’s Dosing Companion (2021) Australian Medicines Handbook Pty Ltd 2021, [Internet] Benzylpenicillin; [Modified July 2021, Cited 18 Oct 2021,] Available from: Benzylpenicillin - AMH Children's Dosing Companion (health.wa.gov.au)
- Thompson MJ, Ninis N, Perera R, Mayon-White R, Phillips C, Bailey L, Harnden A, Mant D, Levin M. Clinical recognition of meningococcal disease in children and adolescents. Lancet. 2006 367:397-403
- Cartwright KAV, Jones DM, Smith AJ, et al. Influenza A and meningococcal disease. Lancet 1991;338:554-557
- Communicable Diseases Network Australia. Guidelines for the early clinical and public health management of meningococcal disease in Australia 2007. http://www.health.gov.au/internet/main/publishing.nsf/content/cda-pubs-other-mening-2007.htm
- National Health and Medical Research Council. Australian Immunisation Handbook, 9th Edition 2008. Department of Health and Ageing. www.health.gov.au/internet/immunise/publishing.nsf/Content/Handbook-meningococcal
- Notification of infectious diseases and related conditions. Government of Western Australia – Department of Health. External website. Cited13 January 2022. Available from: Notification of infectious diseases and related conditions (health.wa.gov.au)
This document can be made available in alternative formats on request for a person with a disability.