Posterior tibial nerve block
Disclaimer
These guidelines have been produced to guide clinical decision making for the medical, nursing and allied health staff of Perth Children’s Hospital. They are not strict protocols, and they do not replace the judgement of a senior clinician. Clinical common-sense should be applied at all times. These clinical guidelines should never be relied on as a substitute for proper assessment with respect to the particular circumstances of each case and the needs of each patient. Clinicians should also consider the local skill level available and their local area policies before following any guideline.
Read the full CAHS Emergency Department disclaimer.
|
Aim
To guide PCH Emergency Department (ED) staff in the procedure of posterior tibial nerve block.
Background1,2
Posterior tibial nerve block achieves sensory blockade to the anterior two thirds of the sole of the foot (not including the webspace between the big toe and second toe).
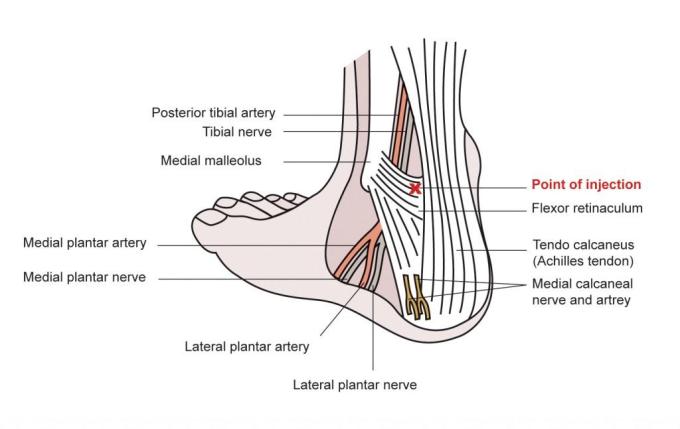
Anatomy
The posterior tibial nerve lies on the medial aspect of the ankle, between the medial malleolus and the Achilles tendon, deep to the flexor retinaculum. The posterior tibial artery can usually be felt behind the medial malleolus. The nerve lies just posterior to this artery (i.e. closer to the Achilles tendon).
- If the artery cannot be palpated, the point of injection should be estimated at the halfway point between the medial malleolus and the Achilles tendon.
- All injections should occur at the level of the upper edge of the medial malleolus.
Pre-Procedure
Indications
- It is useful for painful procedures or injuries involving the sole of the foot (i.e. removal of foreign bodies and wound repair)
- A nerve block avoids the need for painful and difficult infiltration of local anaesthetic into the dense skin and subcutaneous tissue of the sole
Requirements
- The patient needs to be able to cooperate with injections and hold still for the procedure intended.
- Formal consent not required but procedure should be clearly documented.
- A clear explanation of the procedure needs to be provided to the patient.
- Risks need to be explained:
- Pain as the injection is made
- Nerve block might not work
- Bruising and bleeding at the site of injection
- Ensure the patient is in the appropriate treatment area.
Preparation
Equipment and dosing
Needle
- 25-gauge bevelled needle (orange) for the injection
Local anaesthetic
- Dose to be given according to nature of procedure.
- Do not repeat maximum dose more often than every 4 hours.3
- Warm lidocaine (lignocaine) to body temperature (i.e. in your hand) to reduce discomfort.
- Duration: 1-3 hours
Procedure
- Explain the procedure and its purpose to the carer and patient
- Consider topical local anaesthetic e.g. lidocaine (lignocaine) 2.5% with prilocaine 2.5% cream (EMLA®) application over injection site.
- Nitrous oxide can be used as an adjunct during the injection time.
Position
- Position the patient lying down on their side with the foot slightly dorsiflexed.
- Use an assistant to keep the foot in that position.
Technique
- Clean the skin with antiseptic solution
- Identify the point of injection as per illustration above
- Insert perpendicular to the skin just posterior to the artery at the level of the top of the medial malleolus
- If the artery is not palpable, insert at the midpoint between the superior border of the medial malleolus and the Achilles tendon
- Advance until the needle is 1 mm from the tibia
- If paraesthesia is elicited, withdraw 1-2 mm to avoid intraneural injection
- Aspirate before and during injection to avoid arterial injection.
- Inject calculated dose of lidocaine (lignocaine) while slowly withdrawing the needle.
- Wait up to 15 mins and test the sensation in the area concerned before commencing your procedure.
Documentation
- All medication (including local anaesthetic) must be prescribed on the WA paediatric Hospital Medication Chart (pHMC).
- A procedure note should be entered into the patient medical record.
- It is important to document:
- Pre-procedure pain score
- Side of posterior/tibial nerve block
- Use of ultrasound or anatomical landmarks
- Needle type and size
- Local anaesthetic agent and dose
- Immediate complications
- Post nerve block pain scores should be performed and documented in the nursing chart 30 minutes after the procedure.
References
- King C, and Henretic F (2008) Textbook of pediatric emergency procedures. Ch 35. Pg 439-468 Philadelphia: Lippincott Williams and Wilkins.
- Roberts J. (2019) Roberts and Hedges’ Clinical Procedures in Emergency Medicine and Acute Care, Seventh Edition. Boston: Elsevier
- BNF for Children. Medicines Complete. (lignocaine hydrochloride) Last updated: 17 August 2020. Cited: 12 April 2022. Available from: MedicinesComplete — CONTENT > BNF for Children > Drug: Lidocaine hydrochloride (health.wa.gov.au)
- Australian Medicines Handbook [Internet]. Adelaide: AMH; c2022. Lidocaine. Available from: Lidocaine (anaesthesia) - Australian Medicines Handbook (health.wa.gov.au)
| Endorsed by: |
CAHS Drug & Therapeutic Committee |
Date: |
Dec 2025 |
This document can be made available in alternative formats on request for people with disability.