Suprapubic aspiration of urine
Disclaimer
These guidelines have been produced to guide clinical decision making for the medical, nursing and allied health staff of Perth Children’s Hospital. They are not strict protocols, and they do not replace the judgement of a senior clinician. Clinical common-sense should be applied at all times. These clinical guidelines should never be relied on as a substitute for proper assessment with respect to the particular circumstances of each case and the needs of each patient. Clinicians should also consider the local skill level available and their local area policies before following any guideline.
Read the full CAHS clinical disclaimer.
|
Aim
To guide PCH ED staff with performing a suprapubic aspiration of urine (SPA).
Key points
- Suprapubic aspiration of urine is a simple and safe technique for obtaining an uncontaminated specimen of urine in children.1
- SPA is the urine collection method with the lowest contamination rate in infants (1%) compared to in-out catheter specimens (12%) and clean-catch urines (up to 63%).1,2,3
- In stable children, perform before other invasive procedures such as venepuncture and lumbar puncture (in case the child voids).
- Apply Keeping Kids in No Distress (KKIND) principles throughout the procedure.
Indications1
- Children less than 6 months of age who need a urine culture.
- Children less than 1 year old who need repeat urine culture because the previous urine culture is contaminated.
Contraindications
- Passed urine in the previous 1 hour
- Distended abdomen
- Coagulopathy
- Skin infection over puncture site
- Urogenital abnormality
Pre-Procedure1
- If patient has passed urine in the 60 minutes prior to the procedure, feed the patient and wait 30 to 60 minutes.
- Visualising urine in the bladder by ultrasound can increase success rate to 80%.4,5,6
- Prepare all equipment before undoing the nappy; procedure should be done quickly once genitals are exposed.
- Standard aseptic technique with sterile gloves is required.
Preparation
Staff required:
- Doctor to carry out procedure
- Nurse to hold the child throughout procedure
- Assistant to catch urine (if patient passes urine peri-procedure)
Equipment
.jpg)
SPA equipment (photo is for illustrative purposes - all equipment should remain sterile)
- 3 mL or 5 mL syringe
- Alcohol wipe
- 23 gauge needle
- Sterile gloves
- Urine specimen container (yellow top)
- Dressing
Medications
- Sucrose maybe given to infants prior to the procedure.
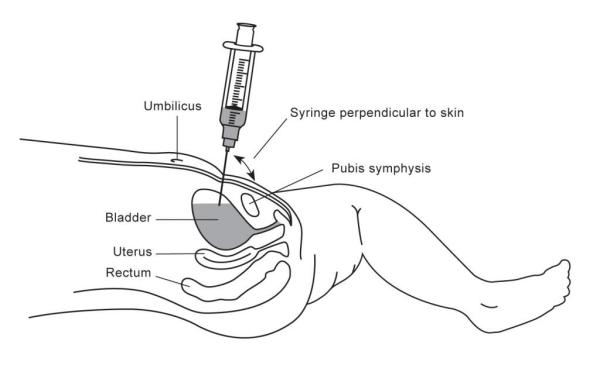
Positioning and technique
- Perform hand hygiene before touching the patient
- Position the child supine
- Nurse holds the child steady in a ‘frog leg’ position or supine with legs extended. An assistant should be ready to catch urine with an open urine specimen jar if the patient passes urine.
Check the bladder size / volume using one of the following 3 methods6,7,8:
- Curvilinear ultrasound probe to check bladder volume:
- Transverse view, depth (D) 2-3 cm or Transverse diameter (T) 3.5 cm (recommended method) or
- Use of ultrasound increases success rate of SPA from 50% to >80%
- Bladder scanner (minimum 20mL) - scan 3 times to confirm, or
- Gently percuss the bladder; fundus should be 1-2 finger breadths above the pubic symphysis (PS).1,9
Procedure1,10
- Standard aseptic no touch technique should be used throughout the procedure.
- Clean the skin from the pubis to umbilicus in a circular motion 5 cm diameter with an alcohol wipe.
- Perform hand hygiene and don sterile gloves.
- Insert the needle (attached to the syringe) perpendicular to the skin at 1-2 cm superior to the pubic symphysis (the suprapubic crease level) in the midline:

- Aspirate gently after the needle pierces the skin. Aspirate as you advance, as well as when you withdraw the needle.
- Advance the needle 2-3 cm deep if needed (i.e., whole length of the 23G needle). Stop advancing needle once urine is aspirated.
- If urine is not obtained, partially withdraw the needle to just below the subcutaneous layer and redirect it slightly cephalad while aspirating. If still unable to obtain urine, partially withdraw and redirect slightly caudally while aspirating.
- The procedure should be abandoned if still unsuccessful and an alternative method of urine collection should be considered.
- Further attempts at SPA should be at the discretion of the Senior Doctor on duty.
- Withdraw needle when adequate volume is obtained, or no further urine can be aspirated.
- Place dressing over puncture site.
- Transfer urine from syringe to yellow top specimen jar. If adequate volume of urine obtained, save 0.5 mL for urine dipstick analysis.
- Remove gloves and perform hand hygiene.
Post-Procedure
Patient
Routine observations and care.
Urine Specimen
- Label specimen jar with patient details and time of specimen collection.
- Place urine sample with a completed pathology form requesting microscopy, culture and sensitivities (M,C&S) in a specimen bag. Clearly identify specimen on the pathology request form as a Suprapubic aspirate sample.
- Send the sample and request form to PathWest specimen reception as soon as possible.
Complications1,10
Complications of SPA are rare but may include:
- Transient, gross or microscopic haematuria
- Intestinal perforation (rarely leads to peritonitis)
- Bladder haematuria
- Abdominal wall abscess
Bibliography
- Bajaj L, Bothner J. Urine collection techniques in infants and children with suspected urinary tract infection. UpToDate. Last updated August 2022. Accessed 24/08/2023
- Tosif S, Baker A, Oakley E, Donath S, Babl FE. Contamination rates of different urine collection methods for the diagnosis of urinary tract infections in young children: an observational cohort study. J Paediatr Child Health. 2012;48(8):65
- Eliacik K, Kanik A, Yavascan O, Alparslan C, Kocyigit C, Aksu N, et al. A Comparison of Bladder Catheterization and Suprapubic Aspiration Methods for Urine Sample Collection From Infants With a Suspected Urinary Tract Infection. Clinical Pediatrics. 2015 2016/08/01;55(9):819-24. https://doi.org/10.1177/0009922815608278
- Gochman RF, Karasic RB, Heller MB. Use of portable ultrasound to assist urine collection by suprapubic aspiration. Ann Emerg Med. 1991;20(6):631.
- Chu RW, Wong YC, Luk SH, et al. Comparingsuprapubicurineaspiration under real-time ultrasound guidance with conventional blind aspiration. Acta Paediatrica. 2002; 91:512–516.
- Munir V, Barnett P, South M. Does the use of volumetric bladder ultrasound improve the success rate of suprapubic aspiration of urine? Pediatric Emergency Care. 2002 Oct; 18(5):346-9.
- Bevan C, Bakhit J, Stock A, Babl F. What measurements on real time ultrasound (RTUS) will predict a successful suprapubic aspiration? Journal of Paediatrics and Child Health. 2011;47(SUPPL. 2):2. English
- Buntsma D, Stock A, Bevan C, Babl FE. Success rate of BladderScan-assisted suprapubic aspiration. EMA - Emergency Medicine Australasia. 2012;24(6):647-51. English.
- Porter FN. Percussion as aid to suprapubic aspiration. Archives of Disease in Childhood. 1988 August; 63(8): 998.
- Abbott GD, Shannon FT. How to aspirate urine suprapubically in infants and children. Clinical Pediatrics. 1970; 9:277.
| Endorsed by: |
Co-director, Surgical Services (Nursing) |
Date: |
Oct 2023 |
This document can be made available in alternative formats on request for a person with a disability.