Haematuria
Disclaimer
These guidelines have been produced to guide clinical decision making for general practitioners (GPs). They are not strict protocols. Clinical common-sense should be applied at all times. These clinical guidelines should never be relied on as a substitute for proper assessment with respect to the particular circumstances of each case and the needs of each patient. Clinicians should also consider the local skill level available and their local area policies before following any guideline.
|
|
If the child is systemically unwell or has an abdominal mass, present to the nearest Emergency Department
|
Introduction
Microscopic haematuria is a common finding in children (>10 RBC/microlitre) and can only be detected by urinalysis as the urine colour remains normal.1, 2
Presentation
|
Isolated microscopic haematuria
|
Microscopic haematuria without clinical symptoms or any other abnormalities. Resolves spontaneously.
|
|
Persistent microscopic haematuria
|
Three urine samples collected >1 week apart with microscopic haematuria. Common causes include glomerulonephritis, thin basement membrane disease, and hypercalciuria.
|
|
Microscopic haematuria with proteinuria
|
Microscopic haematuria with proteinuria (first void urine PCR greater than upper limit of normal for age). May indicate clinically meaningful kidney disease such as glomerulonephritis requiring treatment, Alport syndrome, and nephrotic syndrome.*
|
|
Symptomatic microsopic haematuria
|
Microscopic haematuria with urinary or systemic symptoms. Causes include urinary tract infection, urethritis, renal calculi, and vasculitis.
|
*Microscopic haematuria is common in children with nephrotic syndrome. Children with oedema plus nephrotic range proteinuria (protein-to-creatinine ³200 mg/mmol or ³3+ on dipstick) plus a low serum albumin (less than 25 g/L) should follow the nephrotic syndrome pathway (Nephrotic Syndrome Management).
History
- Previous history of haematuria
- Symptoms of infection: dysuria, frequency, pain, fever
- Systemic symptoms: fatigue, fever, oedema, rash, arthralgia, haemoptysis, epistaxis
- Recent surgery, trauma or exercise
- Family history of haematuria, proteinuria, kidney disease, renal stones, hearing loss
Examination and investigations
- Anthropometric measurements
- Blood pressure
- Weight
- Height
- Examination for oedema and signs of vasculitis (e.g. rashes, aphthous ulcers, scleritis, serositis, arthritis)
- Urinalysis
- Urine MC&S and protein-to-creatinine ratio (first morning) if proteinuria on dipstick
- Urine calcium-to-creatinine ratio
- Blood tests
- FBP
- UEC
- CMP
- LFT
- If patient has proteinuria or signs concerning for vasculitis consider CRP, ESR, C3/C4, ANA, dsDNA, ASOT and anti-DNase, and ANCA
- Renal tract ultrasound
Haematuria with any of these ‘red flag’ symptoms should be discussed with a Paediatrician or Nephrologist:
- Significant proteinuria
- Elevated serum creatinine
- Hypertension
- Fluid overload
Pre-referral management
Table 1: Management of children presenting with haematuria1
When to refer
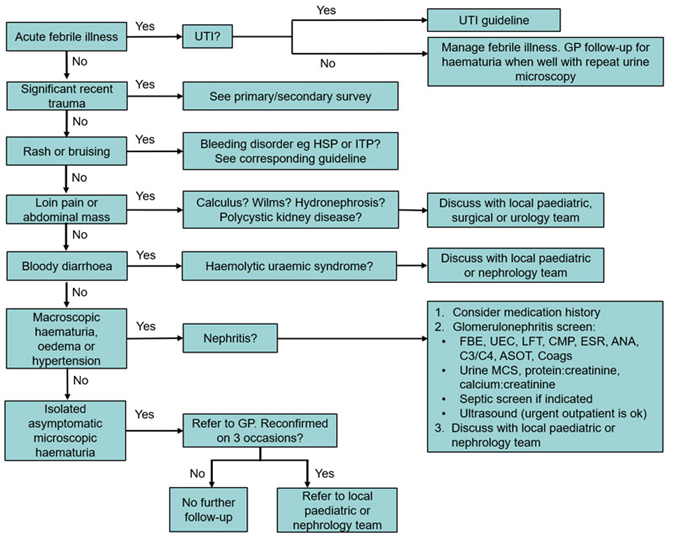
- Persistent microscopic haematuria (see above flowchart) or microscopic haematuria with proteinuria
- Ensure relevant investigations are completed
- If the initial screen and assessment are unrevealing, it is likely the patient will be returned back to their GP for ongoing monitoring (annual BP and urinalysis)
- Haematuria with any of the “red flags” should be discussed with Paediatrics or Nephrology as it may require more urgent review
How to refer
- Routine non-urgent referrals from a GP or a Consultant should go to the Central Referral Service. Routine non-urgent referrals from private hospitals go to the PCH Referral Office (Fax: 6456 0097 or email PCH.Referrals@health.wa.gov.au).
- Urgent referrals (less than seven days) go to the PCH Referral Office. Please call Perth Children’s Hospital Switch on 6456 222 to discuss referral with the on-call Renal specialist.
Essential information to include in your referral
- History, BP and clinical examination
- Results of all investigations
References
- The Royal Children's Hospital Melbourne. Clinical Practice Guidelines: Haematuria [Internet]. Rch.org.au. 2019. Available from: https://www.rch.org.au/clinicalguide/guideline_index/Haematuria/ [accessed 17 November 2022]
- Boyer, G. O., Niaudet, P., Wilkie, L. Evaluation of microscopic hematuria in children [Internet]. 2020 [cited 17 Nov 2022]. Available from: https://www-uptodate-com.pklibresources.health.wa.gov.au/contents/evaluation-of-microscopic-hematuria-in-children?search=haematuria%20paediatric&source=search_result&selectedTitle=2~150&usage_type=default&display_rank=2
| Reviewer/Team: |
Nephrology Department |
Endorsed date: |
May 2023 |
This document can be made available in alternative formats on request for a person with a disability.