Seizure - First presentation
Disclaimer
These guidelines have been produced to guide clinical decision making for the medical, nursing and allied health staff of Perth Children’s Hospital. They are not strict protocols, and they do not replace the judgement of a senior clinician. Clinical common-sense should be applied at all times. These clinical guidelines should never be relied on as a substitute for proper assessment with respect to the particular circumstances of each case and the needs of each patient. Clinicians should also consider the local skill level available and their local area policies before following any guideline.
Read the full PCH Emergency Department disclaimer.
|
Aim
To guide PCH Emergency Department (ED) staff with the assessment and management of a first seizure. presentation.
Definition
- A seizure is the physical and behavioural changes that occur after an episode of abnormal activity in the brain or part of the brain.
- It is a symptom not a diagnosis.
- Epilepsy is the enduring predisposition towards having recurrent epileptic seizures.
Background
- By the age of 16 years, approximately 1% of the population will have suffered a seizure without a fever.1,2,3
- Recurrence risk:2,3
- 25% will have a second afebrile seizure in the next year
- 45% will have a second afebrile seizure in the next 14 years.
Assessment
History
General history including:
- Time, setting and precipitants
- Neurological state and behaviour prior to seizure
- Description of seizure activity including focal features, eye movements and continence
- Duration of seizure
- Fever
- Headache and/or photophobia
- Recent trauma
- Poisons / drug ingestion
- Co-morbidities e.g. ventriculoperitoneal (VP) shunt
- Developmental history
- Determine if the child has had a vaccination in the past 14 days. If so, a WAVSS WA Vaccine Safety Surveillance: Adverse Reaction Reporting Form needs to be completed. Refer to About Western Australia - SAFEVAC Reporting.
Examination
- Systems examination including full neurological examination
- Assess for meningism
Investigations
All children presenting with a paroxysmal event must have
Additional investigation is only required if concerns (seek ED Senior Doctor advice). Consider -
- Urea, electrolytes and creatinine (UEC), Calcium, Magnesium, Phosphate.
- Computerised Tomography (CT) - if focal or traumatic.
- Lumbar Puncture – if infective concerns, and intracranial lesion excluded.
- Metabolic screen – if hepatosplenomegaly or developmental concerns
- EEG and MRI Brain – usually arranged by General Paediatric team if required.
Differential diagnoses
Febrile convulsion
|
Febrile with viral features
|
Meningoencephalitis
|
Unwell, irritable, vomiting, neck stiffness
|
Hypoglycaemia
|
Reduced intake, sweating, pallor
|
Breath holding
|
Preceded by crying
|
Syncope/cardiac
|
Pallor, loss of tone, palpitations
|
Stroke
|
Focal features, bleeding or thrombotic risk
|
Migraine
|
Preceded by nausea, vomiting, visual change, headache
|
| Reflux |
Back arching, retained consciousness
|
| Panic attack |
Hyperventilation, paraesthesia
|
| Functional seizures |
Prolonged duration, fluctuating course, asynchronous movements, rapid recovery, eyes forced shut
|
Management
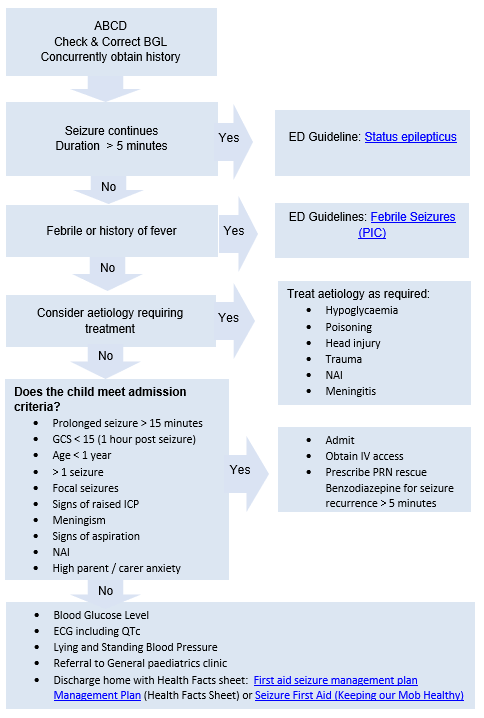
- Most seizures will self-terminate within 5 minutes. Those that last longer are likely to require treatment to terminate. See First Seizure Flowchart below.
- If a seizure is still in progress on arrival to the Emergency Department, treatment should commence as per ED Guideline: Status epilepticus.
- Antiepileptic medication should not be prescribed for a first unprovoked seizure in ED. Many children who experience two or more unprovoked seizures will start antiepileptic medications in outpatients.
Admission criteria
- Prolonged seizure > 15 minutes
- Glasgow Coma Score < 15 (1 hour post seizure)
- Atypical febrile convulsion
- Age < 1 year
- > 1 seizure
- Focal seizures
- Signs of raised intracranial pressure (ICP)
- Meningoencephalitis
- Signs of aspiration
- Non accidental injury (NAI)
- High parental / carer anxiety
Discharge criteria5
- Arrange referral to General Paediatric Clinic.
- Parents should be taught how to recognise further seizures
- Parents should be warned that all children or adolescents who have had seizures should be supervised when bathing, swimming, riding a bicycle on the road, and should avoid tree climbing.
- Parents should be advised of first aid measures and given parent information sheet - First Aid for Seizures or Seizure First Aid (Keeping our Mob Healthy)
- Parents should be advised to reattend ED if further seizures whilst waiting for their General Paediatric Clinic appointment.
References
- Hirtz D, Berg A, Bettis D, Camfield C, Camfield P et al; Practice Parameter: Treatment of the Child with a First Unprovoked Seizure: Report of the Quality Standards Subcommittee of the American Academy of Neurology and the Practice Committee of the Child Neurology Society. Quality Standards Subcommittee of the American Academy of Neurology, Practice Committee of the Child Neurology Society Neurology. 2003;60(2):166.
- Arthur TM, deGrauw TJ, Johnson CS, Perkins SM, Kalnin A, et al; Seizure recurrence risk following a first seizure in neurologically normal children. Epilepsia. 2008; 49(11):1950.
- Shinnar S, Berg AT, MoshéSL, Petix M, Maytal J, Kang H, Goldensohn ES, Hauser. Risk of seizure recurrence following a first unprovoked seizure in childhood: a prospective study. Pediatrics. 1990;85(6):1076-85.
- Wilfong A. Seizures and Epilepsy: Initial Treatment and Monitoring. UpToDate: Wolters Kluwer; Updated Dec 2024. Accessed 15/04/2025.
- Jones KEA, Howells R, Mallick AA, et al. NICE guideline review: Epilepsies in children, young people and adults NG217. Archives of Disease in Childhood - Education and Practice 2023;108:416-421.
| Endorsed by: |
CPAC |
Date: |
May 2025 |
This document can be made available in alternative formats on request for a person with a disability.