Solitary Kidney
Disclaimer
These guidelines have been produced to guide clinical decision making for general practitioners (GPs). They are not strict protocols. Clinical common-sense should be applied at all times. These clinical guidelines should never be relied on as a substitute for proper assessment with respect to the particular circumstances of each case and the needs of each patient. Clinicians should also consider the local skill level available and their local area policies before following any guideline.
|
|
If the child is systemically unwell or has an abdominal mass, present to the nearest Emergency Department
|
Introduction
Solitary functioning kidney (SFK) is a low-risk congenital anomaly, which in most cases can be managed in general practice (GP). In the general population, congenital SFK is relatively rare with an estimated prevalence of 1 in 2000 newborns1. SFK is a condition of low nephron mass. The concurrence of other conditions known to reduce nephron mass (such as prematurity or intra-uterine growth restriction, and moderate to severe acute kidney injury), further increase the degree of hyperfiltration in the residual renal mass. Other comorbidities such as diabetes mellitus and hypertension, increasingly common in the paediatric population, can lead to an exacerbation of hyperfiltration injury in children already with low nephron mass.
The most common causes for SFK include:
- Congenital anomalies of the kidney and urinary tract (CAKUT) including:
- contralateral multicystic dysplastic kidney (MCDK)
- contralateral aplastic/dysplastic kidney with very low or minimal function
- entirely absent (agenesis) contralateral kidney at birth
- Surgical nephrectomy of one kidney due to malignancy such as Wilm’s tumour
Contralateral MCDK is a common cause of a SFK. Just over half of children with MCDK will completely involute, most within 3 years; less likely if they are greater than 6cm. Failure to involute is not an indication for surgical removal
Most children with a healthy SFK do well, with normal renal function throughout most of their lives. However, there is a subset in whom further abnormalities in the SFK become evident with age (e.g., dysplasia not observed on early scan), which can lead to chronic kidney disease (CKD) in the medium-to-long-term. For this reason, the screening below is recommended, along with incorporating kidney health checks into routine care at the GP/primary care provider as detailed.
History
- Events causing solitary kidney (congenital vs. surgical)
- Antenatal and perinatal history (e.g. gestational age, birth weight, neonatal course)
- Previous acute kidney injury history, if any
- History of nephrotoxin exposure if any (e.g. NSAID use, chemotherapy)
- Symptoms and history of urinary tract infection: dysuria, frequency, pain, fever
- Hydration and voiding history
- Family history of haematuria, proteinuria, kidney disease and renal stones
Examinations and investigations
- Anthropometric measurements
- Blood pressure percentile4
- Weight percentile
- Height percentile
- General screening cardiac and abdominal exam
- Genitourinary exam (e.g. look for ambiguous genitalia and undescended testes)
- Urinalysis
- Urine MC&S and protein-to-creatinine ratio (first morning) if proteinuria on dipstick
- Blood tests including: FBP, UEC, CMP, LFT
- Renal tract ultrasound (if not done at the time of diagnosis of solitary kidney)
Solitary kidney with any of these “red flags” should be discussed more urgently with a Paediatric Nephrologist:
- Nephrotic range proteinuria (spot urine protein:creatinine >200mg/mmol)
- Macroscopic haematuria
- Elevated serum creatinine
- Stage II Hypertension4 or above
- Renal stones
- Hydronephrosis
- Pyelonephritis
Pre-referral management
|
All patients require the following annually:
- BP-with appropriately sized BP cuff for age/size4
- Urinalysis and protein-to-creatinine ratio (first morning) if proteinuria on dipstick
|
|
In addition the following procedures are required, depending on the patient’s age:
|
|
2-3 months old
|
- Renal tract USS (if antenatally detected and no postnatal ultrasound has been done)
|
|
1 year old
|
- Renal tract USS
- In males, a routine genitourinary exam to ensure bilateral testes are descended and of normal size
|
|
5 years old
|
- Renal tract USS
- Screening bloods: FBP, UEC, CMP, LFT
|
|
10 years old
|
- Renal tract USS
- In females, the ultrasound at 10 years of age should include views of the uterus and ovaries
|
|
15 years old
|
|
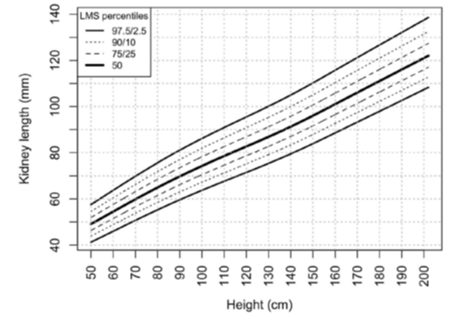
Paediatric normative renal length percentiles based on height/length6
Other recommendations
Daily hydration target:
- Toddler age – 750mL or more fluid per day
- School age – 1L or more fluid per day
- Adolescent & adult – 1.5-2L or more fluid per day
- Seek medical attention should there be acute illness preventing oral hydration.
Avoid NSAIDS
- At high and regular dosage (e.g., Ibuprofen not to exceed 10mg/kg/dose for those under 40kg, or 400mg/dose for those >40kg, with maximum one dose per day for less than 3 consecutive days)
- Avoid NSAIDS at any dose if not hydrating well
Lifestyle:
- Encourage exercise and aim for a healthy weight
- No smoking
- No binge alcohol drinking
Solitary kidney and sport
Solitary kidney patients do not need to avoid contact sport from the renal perspective. We recommend considering a kidney guard for high-risk activities, such as motorbike riding, BMX, kick boxing, horse riding, AFL (high-school or older). Evidence has shown that the risk of renal injury as a result of contact/collision sport is less than that of other risks considered acceptable by the general community, for example head injury and spinal cord injury5. Furthermore, the benefits of physical activity, such as decreasing the risk of obesity, diabetes, and hypertension, outweigh the relative risk of a kidney injury. For more information, please refer to useful resources (see below).
When to refer
Patients with the below features should be referred to the Nephrology Department at PCH
- Patients with any of the aforementioned “red flag” features should be discussed with a paediatrician or paediatric nephrologist within 7 days
- Significant proteinuria (PCR>20mg/mmol on a first morning urine sample)
- Persistent (on three occasions) microscopic haematuria
- Hypertension4
- Abnormal sonographic features in the solitary kidney, including lack of growth above 95th centile for patient height
- Family history of kidney failure in the 4th decade of life or younger
- History of prematurity at birth <32/40 or IUGR <2.5 kg
In the absence of features to suggest concern, patients with SFK can be managed by their general practitioner or paediatrician using the outlined schedule above, which is the same as our routine care. PCH Renal Specialists can provide advice or review ultrasound images.
How to refer
- Routine non-urgent referrals from a GP or a Consultant should go to the Central Referral Service. Routine non-urgent referrals from private hospitals go to the PCH Referral Office (Fax: 6456 0097 or email PCH.Referrals@health.wa.gov.au)
- Urgent referrals (less than seven days) go to the PCH Referral Office. Please call Perth Children’s Hospital Switch on 6456 222 to discuss referral with the on-call Renal specialist
Essential information to include in your referral
- History, BP and clinical examination
- Most recent ultrasound report with images uploaded to Enterprise Medical Imaging Platform.
References
- La Scola C, Ammenti A, Bertulli C, Bodria M, Brugnara M, Camilla R, Capone V, Casadio L, Chimenz R, Conte ML, Conversano E, Corrado C, Guarino S, Luongo I, Marsciani M, Marzuillo P, Meneghesso D, Pennesi M, Pugliese F, Pusceddu S, Ravaioli E, Taroni F, Vergine G, Peruzzi L, Montini G. Management of the congenital solitary kidney: consensus recommendations of the Italian Society of Pediatric Nephrology. Pediatr Nephrol. 2022 Sep;37(9):2185-2207.
- Aslam M, Watson AR; Trent & Anglia MCDK Study Group. Unilateral multicystic dysplastic kidney: long term outcomes. Arch Dis Child. 2006 Oct;91(10):820-3.
- Hains DS, Bates CM, Ingraham S, Schwaderer AL. Management and etiology of the unilateral multicystic dysplastic kidney: a review. Pediatr Nephrol. 2009
- Clinical Practice Guidelines : Hypertension in children and adolescents (rch.org.au)
- Psooy K, Franc-Guimond J, Kiddoo D, Lorenzo A, MacLellan D. Canadian Urological Association Best Practice Report: Sports and the solitary kidney - What primary caregivers of a young child with a single kidney should know (2019 update). Can Urol Assoc J. 2019 Oct;13(10):315-317.
- Obrycki, Ł., Sarnecki, J., Lichosik, M. et al. Kidney length normative values in children aged 0–19 years — a multicenter study. Pediatr Nephrol 37, 1075–1085 (2022).
| Reviewer/Team: |
Nephrology Department
|
Last reviewed: |
July 2023 |
|
|
Review date: |
July 2026 |
This document can be made available in alternative formats on request for a person with a disability.