Mallet finger
Disclaimer
These guidelines have been produced to guide clinical decision making for the medical, nursing and allied health staff of Perth Children’s Hospital. They are not strict protocols, and they do not replace the judgement of a senior clinician. Clinical common-sense should be applied at all times. These clinical guidelines should never be relied on as a substitute for proper assessment with respect to the particular circumstances of each case and the needs of each patient. Clinicians should also consider the local skill level available and their local area policies before following any guideline.
Read the full CAHS clinical disclaimer.
|
Aim
To guide PCH Emergency Department (ED) staff with the assessment and management of mallet finger.
Background
- Caused by forceful flexion to the end of an extended finger.
- Most frequently occurs in contact or ball-handling sports such as baseball, football and basketball.
- The terminal extensor tendon on the dorsum of the finger at the distal interphalangeal joint (DIP) is torn, stretched or avulsed.
Assessment
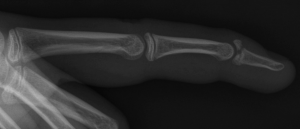
- Pain, swelling (+ / bruising) on the dorsum of the DIP joint.
- Flexed posture of finger tip due to inability to actively extend it.
- Passive (by the examiner) extension is usually possible. Inability to extend DIP passively indicates bony or soft tissue entrapment.
- The degree of DIP angulation often reflects the severity of the tendon disruption.
- Open injuries are rare.

Middle finger with mallet deformity
Investigations
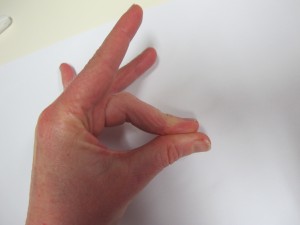
- Request a finger X-ray of the affected digit. This should have PA (posterior-anterior), oblique, and lateral views.
- Look for a dorsal avulsion fracture of the distal phalanx at DIP joint.
X-ray of mallet finger
Management
Open injury, inability to passively extend DIP joint or large fracture > 30% of joint surface
- Call plastics registrar for review and fast the child for possible surgery.
All other closed injuries
- Preferred splint - Stax splint (see below)
- Alternative splint - Zimmer splint (see below )
- if unable to find a suitable size Stax splint or unavailable
- Both splints are designed to splint the DIP joint in hyper-extension but permit PIP joint movement
- Instruct the patient / family to not remove the splint, as even brief DIP joint flexion can delay healing and impair final joint function
- Follow up Plastics Clinic in 1 to 2 days time.
Stax finger splint

|
Dorsal part of Stax splint. note the number that indicates the splint size
|

|
Volar aspect of Stax finger splint
|

|
Fix finger just distal to PIP joint with a small adhesive strip (e.g. Elastoplast)
|

|
Volar aspect of Stax splint
|
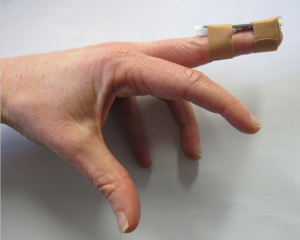
Zimmer splint - Kleinert modified dorsal finger splint (Mexican hat splint)3

|
Zimmer splint (aluminium with foam backed splint) cut to the appropriate length, from the finger tip to just distal to the PIP joint
|

|
Removed middle third of foam padding with scissors. Bend each end of the splint to form a slight concave contour.
|
|
Instruct patient to hold the injured finger in hyperextension.
|
|
Affix splint to dorsum of the digit with two separate tapings, ensuring the DIP joint is held in hyper-extension.
|
References
- Practical Fracture Treatment Fifth Edition. Ronald McRae, Max Esser. Churchill Livingstone, 2008
- Rang's Children's Fractures Fourth edition. Mercer Rang, Maya E. Pring, Dennis Ray Wenger. Wolters Kluwer, 2018
- R. G. Hart et al, The Kleinert modified dorsal splint for Mallet finger fracture. American Journal of Emergency Medicine 2005 (23), 145‐148.
| Endorsed by: |
Nurse Co-Director, Medical Services |
Date: |
Mar 2024 |
This document can be made available in alternative formats on request for a person with a disability.