Fractures - Ankle
Disclaimer
These guidelines have been produced to guide clinical decision making for the medical, nursing and allied health staff of Perth Children’s Hospital. They are not strict protocols, and they do not replace the judgement of a senior clinician. Clinical common-sense should be applied at all times. These clinical guidelines should never be relied on as a substitute for proper assessment with respect to the particular circumstances of each case and the needs of each patient. Clinicians should also consider the local skill level available and their local area policies before following any guideline.
Read the full CAHS clinical disclaimer.
|
Refer to Fractures - Overview for General Assessment and Management
Mechanism of injury
- Adduction and inversion of the foot.
Examination
- There is usually localised swelling and tenderness over one or both malleoli.
- There may be clinical deformity of the ankle joint.
- Assess the child’s ability to weight bear after analgesia.
- Assess passive and active movement of the ankle joint.
Imaging
- An ankle X-ray should have anterior posterior (AP), mortise, and lateral views, and include the proximal end of the metatarsals.
- Children under 2 years of age should have AP and lateral views of the full-length tibia and fibula.
- Displaced physeal and triplane fractures may need a Computerised Tomography (CT) scan.
Specific management1
Ankle sprains
- Ankle sprains are more common in older adolescents once their growth plates have fused.
- Be careful of diagnosing ankle sprains in pre-pubescent children, undisplaced Salter-Harris I distal fibula fractures are commonly missed.
- The most common ligament injured is the anterior talofibular ligament – there is maximal tenderness just anterior to the distal fibula.
- Ankle sprains / ligamentous injuries can be managed with simple analgesia, rest, ice, compression and elevation.
- Crutches can be used until the patient can weight bear without a limp, although early mobilisation with analgesia should be encouraged.
- Patients who are unable to weight bear, with no fracture on x-ray should be managed in a Controlled Ankle Motion (CAM) boot and crutches with GP follow up in 7-10 days.
Distal Fibula fractures
Salter Harris I Fractures
- Commonly misdiagnosed as ankle sprains.
- If undisplaced, there may only be soft tissue swelling over the lateral malleolus on X-ray.
- There is maximal tenderness over the lateral malleolus.
- Manage in a CAM boot for 3-4 weeks weight bearing as tolerated.
- No formal follow up is required.
Salter Harris II Fractures
- If undisplaced, manage in a CAM boot for 3-4 weeks weight bearing as tolerated with GP follow up for a repeat X-ray in 7-10 days to ensure no displacement.
- If displaced, manage in a below knee plaster backslab, non-weight bearing with crutches and follow up in Orthopaedic Fracture clinic in 7-10 days.

Minimally displaced Salter-Harris II fracture of distal fibula
Avulsion fractures of Distal Fibula
- Manage in a CAM boot for 3-4 weeks with weight bearing as tolerated.
- No formal follow up is required.
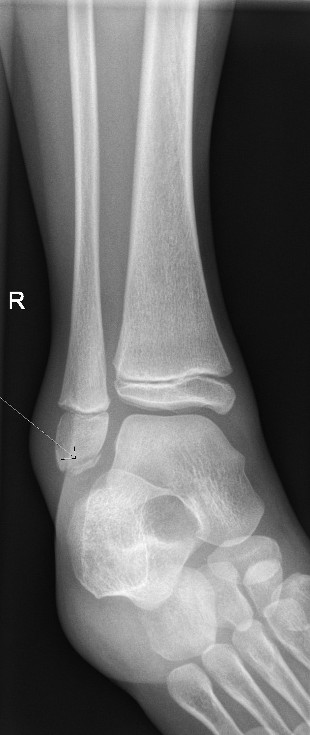
Avulsion of distal fibula
Epiphyseal fracture of distal fibula
- If undisplaced, manage in a CAM boot for 3-4 weeks weight bearing as tolerated with GP follow up. For a repeat X-ray in 7-10 days to ensure no displacement.
- If displaced, manage in a below knee plaster backslab, non-weight bearing with crutches, with follow up in Orthopaedic Fracture clinic in 7-10 days.

Undisplaced epiphyseal fracture of fibula
Distal tibia fractures
Salter-Harris II fractures of the distal tibia
- Often occur in combination with a greenstick fracture of the fibula.
- If undisplaced, manage in a below knee plaster backslab non weight bearing with crutches with follow up in Orthopaedic Fracture clinic in 7-10 days.
- If displaced, refer to the Orthopaedic Team.

Minimally displaced Salter-Harris II fracture of the distal tibia
Salter-Harris III and IV fractures of the distal tibia
- Involves the articular surface of the ankle.
- Refer to Orthopaedic team.

Salter-Harris III fracture of medial malleolus – requires internal fixation
- Tillaux fracture is a lateral Salter-Harris III fracture of the distal tibia (as the medial part of the growth plate fuses first)

Minimally displaced Tilleaux fracture
- Triplane fracture is a combination Salter-Harris II and Tillaux fracture of the distal tibia which occurs in 3 planes.
- Will often need a CT scan to evaluate displacement.

Triplane fracture of distal tibia
References
- Bradman K, Stannage K, O’Brien S, Green, S et al. Randomised controlled trial comparing immobilisation in above-knee plaster of Paris to controlled ankle motion boots in undisplaced paediatric spiral tibial fractures. (2021) Emerg Med J 2021;0:1–7. doi:10.1136/emermed-2020-210299
- McRae R, Max Esser M, Practical Fracture Treatment Fifth Edition, Churchill Livingstone, 2008
- Nelson Textbook of Pediatrics: 21st Edition Kliegman RM, St. Geme J, Blum NJ, Shah SS et al. Publisher: Elsevier 2020
- Rang M, Pring ME, Wenger DR. Kluwer W, Rang's Children's Fractures Fourth edition. Wolters Kluwer, 2018
| Endorsed by: |
Nurse Co-Director, Surgical Services |
Date: |
Mar 2024 |
This document can be made available in alternative formats on request for a person with a disability.