Fractures - Lower leg
Disclaimer
These guidelines have been produced to guide clinical decision making for the medical, nursing and allied health staff of Perth Children’s Hospital. They are not strict protocols, and they do not replace the judgement of a senior clinician. Clinical common-sense should be applied at all times. These clinical guidelines should never be relied on as a substitute for proper assessment with respect to the particular circumstances of each case and the needs of each patient. Clinicians should also consider the local skill level available and their local area policies before following any guideline.
Read the full CAHS Clinical disclaimer
|
See Fractures – Overview for General Assessment and Management
Mechanism of Injury
- Most common mechanism of injury for a lower leg fracture is a fall, resulting in a direct blow or a rotational force.
- Sports injuries and motor vehicle accidents are a common mechanism in older children.
- Toddler’s fractures commonly occur with minimal trauma in the child who is learning to walk and trips over. The mechanism may be trivial and often no injury is recalled by the parents.
Examination
- Tibial shaft fractures will have localised swelling and tenderness with or without clinical deformity. The child will not weight bear on the injured leg.
- Toddler's fractures often have subtle physical findings with minimal swelling and tenderness. Toddlers will favour the injured leg and not want to weight bear.
- Carefully examine the hip, knee and ankle joints to exclude septic arthritis, other injury and other causes of limp.
Imaging
- A tibia / fibula X-ray should have anteroposterior (AP) and lateral views and include the knee and ankle joints.
- Toddler’s fractures may have an initial normal X-Ray or appear as an incomplete vertical or oblique hairline crack in the distal tibia. It is typically seen in only one view. If the initial X-Ray is normal, follow up X-Ray 7-10 days later may show signs of periosteal reaction or healing.
Specific management
Toddler’s Fractures1
- Undisplaced spiral fracture of the tibia
- Common in children < 5 years of age
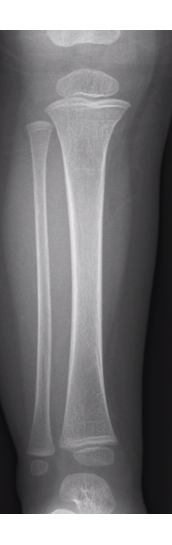
Fracture seen

Toddler fractures are not always apparent as in this X-ray
Suspected Toddler’s Fracture with no Radiological evidence
- Child is limping with a clear history of an injury.
- Possible occult toddler’s fracture.
- Treat with CAM boot for comfort
- Repeat X-ray with GP in 7 days if still not weight bearing.
- Consider alternative diagnosis – foot/hip injury, infective process.
Buckle fractures
Distal tibia buckle fractures
- Manage in a CAM boot weight bearing as tolerated for 3 weeks with no contact sports for a further 3 weeks after splint removal.
- The CAM boot can be removed at night for sleep.
- Give a copy of the Buckle Fracture - Tibia (lower leg) Health Facts sheet to the parent / carer.
- No specific follow up is needed.
Proximal tibia buckle fractures
- Common trampoline injury in younger children.
- Manage in a Richard’s splint (must cover the fracture site) weight bearing as tolerated, with the splint worn day and night for 3 weeks with no contact sports for a further 3 weeks after splint removal.
- Give a copy of the Buckle Fracture - Tibia (lower leg) Health Facts sheet to the parent / carer.
- No specific follow up is needed.
- If the Richard’s splint is too large or does not cover the fracture site, apply an above knee backslab with Orthopaedic Fracture clinic follow up in 1 week.
Proximal tibial buckle fracture
Shaft of tibia / fibula fractures
Undisplaced tibial shaft fractures
- Above knee backslab non weight bearing with crutches and follow up in the Orthopaedic Fracture clinic in 1 week.
Undisplaced fibula shaft fractures
- Rarely need Orthopaedic intervention even if displaced but should be managed in an above knee backslab non weight bearing with crutches and followed up in the Orthopaedic Fracture clinic in 1 week.

Undisplaced transverse fracture of tibia (arrow left)

Spiral fracture of tibia with minimal displacement
Displaced, angulated or shortened tibial shaft fractures
- Refer to the Orthopaedic team for possible reduction.
- Fractures with less than 10 degrees angulation and less than 20% displacement may not require reduction but should be discussed with the Orthopaedic team if there is any doubt.
- High velocity injuries or fractures with significant swelling are at high risk of compartment syndrome and should be referred to the Orthopaedic team for admission.

Oblique comminuted fracture of tibia and fibula

Completely displaced tibial shaft and fibula fracture from a quad bike accident. A high risk of compartment syndrome.
Health information (for carers)
- Refer to Useful Resources
- Advise parents of the signs and symptoms of compartment syndrome.
- Crutches
References
- Bradman et al. Toddler’s Fracture Immobilisation (ToFI) study - A randomised controlled trial comparing immobilisation in above knee plaster of Paris to controlled ankle motion boots in undisplaced paediatric spiral tibial fractures. 2020 (Unpublished).
- McRae R, Max Esser M, Practical Fracture Treatment Fifth Edition, Churchill Livingstone, 2008
- Rang M, Pring ME, Wenger DR. Kluwer W, Rang's Children's Fractures Fourth edition. Wolters Kluwer, 2018
| Endorsed by: |
Co-director Surgical Services (Nursing) |
Date: |
Feb 2024 |
This document can be made available in alternative formats on request for a person with a disability.