Fractures - Knee
Disclaimer
These guidelines have been produced to guide clinical decision making for the medical, nursing and allied health staff of Perth Children’s Hospital. They are not strict protocols, and they do not replace the judgement of a senior clinician. Clinical common-sense should be applied at all times. These clinical guidelines should never be relied on as a substitute for proper assessment with respect to the particular circumstances of each case and the needs of each patient. Clinicians should also consider the local skill level available and their local area policies before following any guideline.
Read the full CAHS Clinical disclaimer
|
See Fractures – Overview for general assessment and management
Mechanism of injury
- Sports accidents with a twisting mechanism, motor vehicle accidents, or direct trauma to the knee.
Examination
- Tenderness of the knee with decreased range of movement and unwillingness to weight bear.
- A large effusion / haemarthrosis is suggestive of an avulsion or ligamentous injury.
- A patella dislocation is often clinically evident with the knee held semi flexed with the patella displaced laterally and superiorly.
- Ability to straight leg raise against resistance should be tested to assess the extensor mechanism (quadriceps tendon, patella, patella tendon).
- In the acute setting, it is often difficult to assess ligamentous laxity / knee instability due to pain and swelling. These patients are immobilised in a Richard’s Splint with crutches and followed up in the Orthopaedic Fracture clinic in 10-14 days when the swelling has reduced.
Imaging
- A knee X-ray should have Anterior Posterior (AP) and lateral views and include the distal third of the femur and proximal third of the tibia and fibula.
- Request patella (skyline) views if fractured patella suspected.
General management
For general assessment and management, see Fractures - Overview.
Specific management
Ligamentous Injuries and Avulsion Fractures
- Ligamentous injuries are uncommon before growth plate closure.
- The medial collateral and anterior cruciate ligaments are most commonly injured.
- Anterior cruciate ligament (ACL) injury is often associated with avulsion of the tibial spine.
- Significant avulsion injuries should be discussed with the Orthopaedic team.
- Immobilise the knee in an appropriately sized Richard’s Splint with crutches and follow up in the Orthopaedic Fracture clinic in 10-14 days.

Avulsion of tibial spine (insertion of cruciate ligament)

Avulsion of fracture of lateral tibial condyle (Segond Fracture). Associated with ACL and medial meniscus injuries
Tibial tuberosity fractures
- Avulsion fracture of the tibial tuberosity is seen in adolescents when the quadriceps contracts violently and suddenly e.g. high jump.
- There is usually a history of Osgood Schlatter disease.
- Refer these to the Orthopaedic team for possible operative management.

Avulsion of tibial tuberosity with superior displacement. Note high riding patella (above).
Physeal fractures around the knee
- Distal femoral and proximal tibial physeal fractures have a high incidence of growth sequelae and should be referred to the Orthopaedic team urgently for reduction and immobilisation.
- The popliteal structures are tethered around the point of the proximal tibial physis and careful neurovascular examination should be performed.
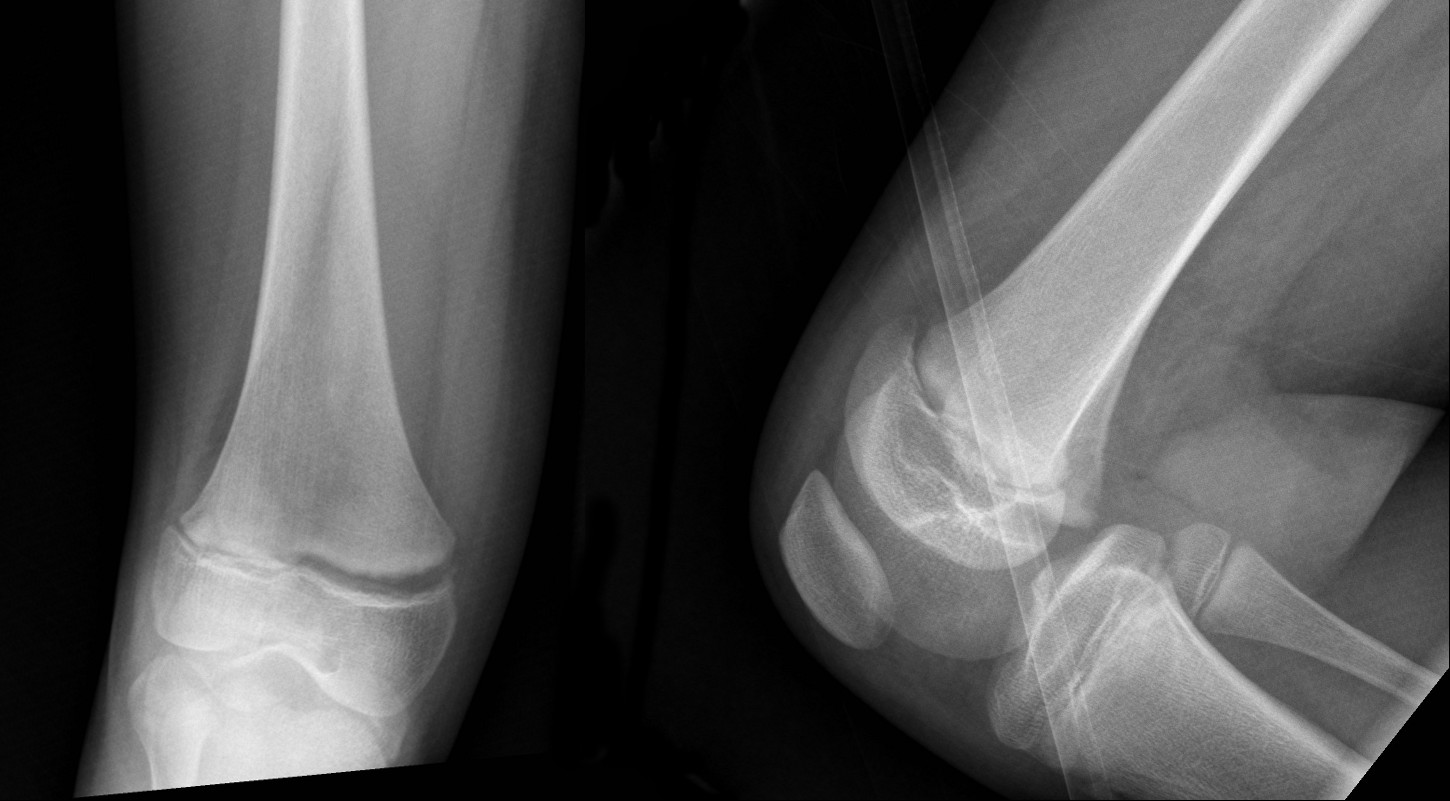
Distal femoral physeal fracture – widened physis with mild anterior displacement. – Salter-Harris I fracture (above).
Patella fractures
- Transverse, avulsion or sleeve fractures are more common in adolescents than young children.
- Non-displaced fractures are immobilised in a Richard’s splint and crutches with follow up in the Orthopaedic Fracture clinic in 10-14 days.
- Displaced patella fractures should be referred to the Orthopaedic team.

Patella sleeve fracture. The patient clinically had difficulty extending knee (above)
Patella dislocations
- The patella usually dislocates laterally and is obvious clinically.
- Dislocations should be reduced in the Emergency Department (ED) after analgesia and procedural sedation (Nitrous oxide - PCH Medications Manual (internal WA Health only) is usually sufficient).
- The knee is extended (straightened) whilst pushing the patella in a medial direction.
- Post reduction X-Rays should be taken to exclude osteochondral fracture.
- Immobilise in a Richard's splint and crutches with follow up in the Orthopaedic Fracture clinic in 10-14 days.
Knee dislocations
- Femorotibial joint dislocations are rare in children but have a high incidence of neurovascular injury.
- They result from high energy trauma (motor vehicle accidents) and may spontaneously reduce before arrival to hospital but are still associated with neurovascular injury.
- Refer all to the Orthopaedic team urgently.
References
- McRae R, Max Esser M, Practical Fracture Treatment Fifth Edition, Churchill Livingstone, 2008
- Rang M, Pring ME, Wenger DR. Kluwer W, Rang's Children's Fractures Fourth edition. Wolters Kluwer, 2018
| Endorsed by: |
Co-director Surgical Services (Nursing) |
Date: |
Mar 2024 |
This document can be made available in alternative formats on request for people with disability.