Fractures - Clavicle
Disclaimer
These guidelines have been produced to guide clinical decision making for the medical, nursing and allied health staff of Perth Children’s Hospital. They are not strict protocols, and they do not replace the judgement of a senior clinician. Clinical common-sense should be applied at all times. These clinical guidelines should never be relied on as a substitute for proper assessment with respect to the particular circumstances of each case and the needs of each patient. Clinicians should also consider the local skill level available and their local area policies before following any guideline.
Read the full CAHS clinical disclaimer.
|
See Fractures – Overview for General Assessment and Management
Mechanism of injury
- Fall onto outstretched hand or direct impact to the shoulder (from fall or sporting collision)
- In neonates, it may be the result of birth injury – the clavicle is the most common obstetric fracture site.
- Infants may present with reluctance to use an arm without a good history of trauma.
Examination
- There is usually tenderness or swelling along the clavicle.
- Assess skin integrity looking for blanching or tenting (ensure the skin moves freely over the injury site).
- After high force trauma, medial clavicle fractures and upper rib fractures may be associated with injury of the great vessels or brachial plexus. Careful neurovascular examination of the ipsilateral arm should be performed.
- Acromioclavicular joint disruption will have tenderness and swelling over the AC joint.
Imaging
- Request “clavicle XR”, rather than “shoulder XR” – AP (anterior posterior) and 15-degree cephalic tilt will be done to show displacement.
- A CT (Computerised Tomography) scan may be required for medial sternoclavicular dislocation.
Specific management
Middle third fractures
- Exclude tenting of the skin.
Minimally displaced middle third fractures

Minimally displaced middle third clavicle fracture
Significantly displaced middle third fractures
- Broad arm sling with referral to the Orthopaedic Fracture Clinic in 1-2 weeks’ time due to risk of non-union.
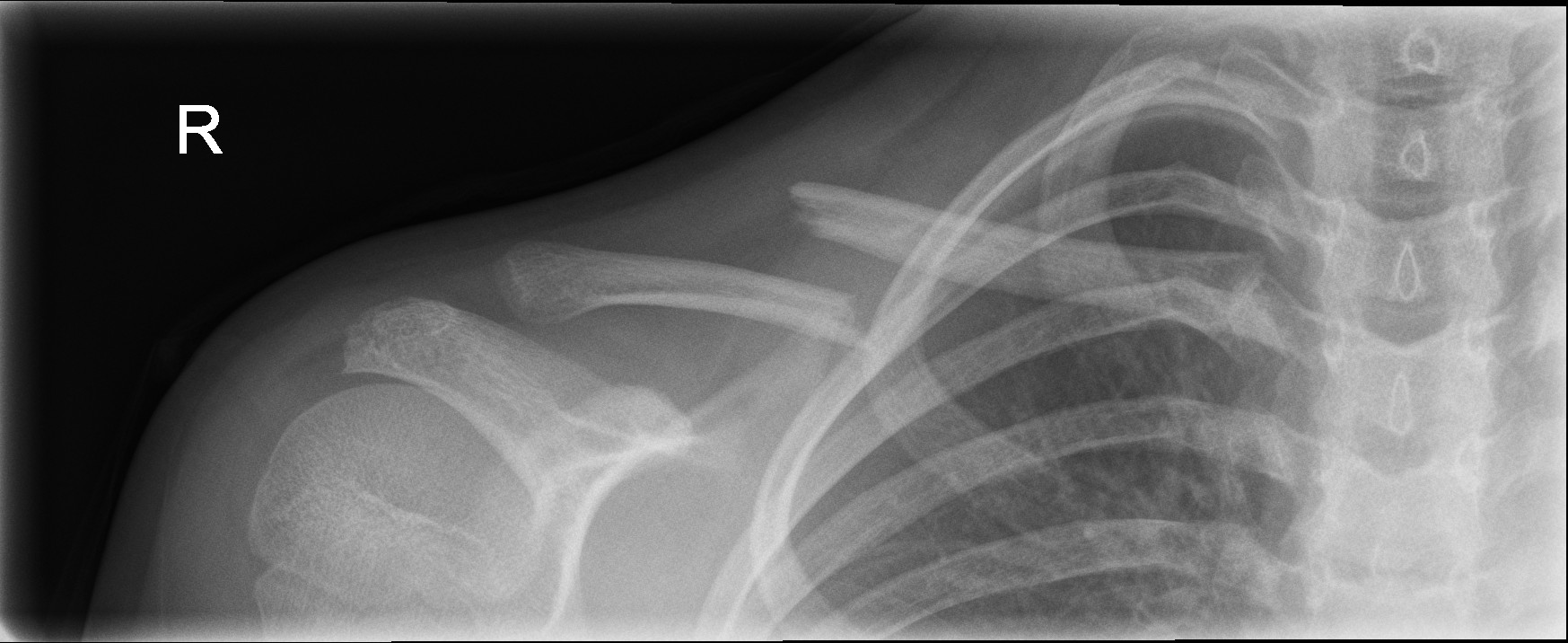
Displaced middle third clavicle fracture
Medial and Lateral Third Fractures
- Discuss with Orthopaedics.

Lateral third clavicle fracture
Acromioclavicular Joint Disruption
- Immobilise in a broad arm sling and refer to the Orthopaedic Fracture Clinic in 1-2 weeks’ time.
Neonatal Clavicle Fractures
- Apply a simple swathe for 2 weeks.
References
- Rang M, Pring ME, Wenger DR. Kluwer W, Rang's Children's Fractures Fourth edition. Wolters Kluwer 2018
- McRae R, Max Esser M, Practical Fracture Treatment Fifth Edition, Churchill Livingstone, 2008
| Endorsed by: |
Co-director Surgical Services (Nursing) |
Date: |
Mar 2024 |
This document can be made available in alternative formats on request for a person with a disability.