Fractures - Humerus
Disclaimer
These guidelines have been produced to guide clinical decision making for the medical, nursing and allied health staff of Perth Children’s Hospital. They are not strict protocols, and they do not replace the judgement of a senior clinician. Clinical common-sense should be applied at all times. These clinical guidelines should never be relied on as a substitute for proper assessment with respect to the particular circumstances of each case and the needs of each patient. Clinicians should also consider the local skill level available and their local area policies before following any guideline.
Read the full CAHS Clinical disclaimer
|
See Fractures – Overview for General Assessment and Management
Mechanism of injury
- Fall or direct trauma to the proximal humerus.
- Spiral fractures are the result of a twisting injury and may be secondary to non-accidental injury especially in children < 2 years of age.
Examination
- Swelling and mild tenderness of the upper arm with reluctance to move.
- Obvious deformity and shortening may be present with displaced fractures.
- Look for weakness in thumb or wrist extension and sensory loss in the web space between thumb and index finger.
Imaging
- A humerus X-ray should have anteroposterior (AP) and lateral views and include the shoulder and elbow joints.
Specific management
Proximal Humerus Fractures
- Younger children are prone to buckle fractures of the proximal humerus.
- Adolescents are more likely to have Salter-Harris fractures around the physis.
- The degree of angulation is usually not an issue. This will correct with gravity and remodelling.
Proximal humerus fractures with < 50% displacement
- Collar and cuff with the elbow at 90 degrees and Orthopaedic Fracture clinic follow up in 1 week.
Proximal humerus fractures with > 50% displacement
- Discuss with Orthopaedic team for further management.

Above: Buckle fracture of proximal humerus

Above: Proximal humerus fracture with 40 degrees of angulation

Above: Salter-Harris II fracture of proximal humerus
Shaft Fractures
- Shaft fractures of the humerus are less common than proximal or distal (supracondylar) fractures.
- Transverse fractures generally occur from a direct blow and spiral fractures from a twisting mechanism.
- Consider non-accidental injury in younger children with spiral fractures. Discuss with senior ED doctor and Child Protection Unit if concern for NAI.
Shaft fractures with minimal angulation (< 10 degrees in adolescents and < 20 degrees in younger children)
- Collar and cuff with the elbow at 90 degrees and Orthopaedic Fracture Clinic follow up in 1 week.
- A U-slab is an alternative to protect the fracture site – discuss with senior ED doctor or Orthopaedics team if there is significant displacement.
Shaft fractures with > 10 degrees of angulation, complete displacement or radial nerve deficits
- Discuss with Orthopaedic team for further management.

Above: Complete fracture of shaft of humerus with mild displacement
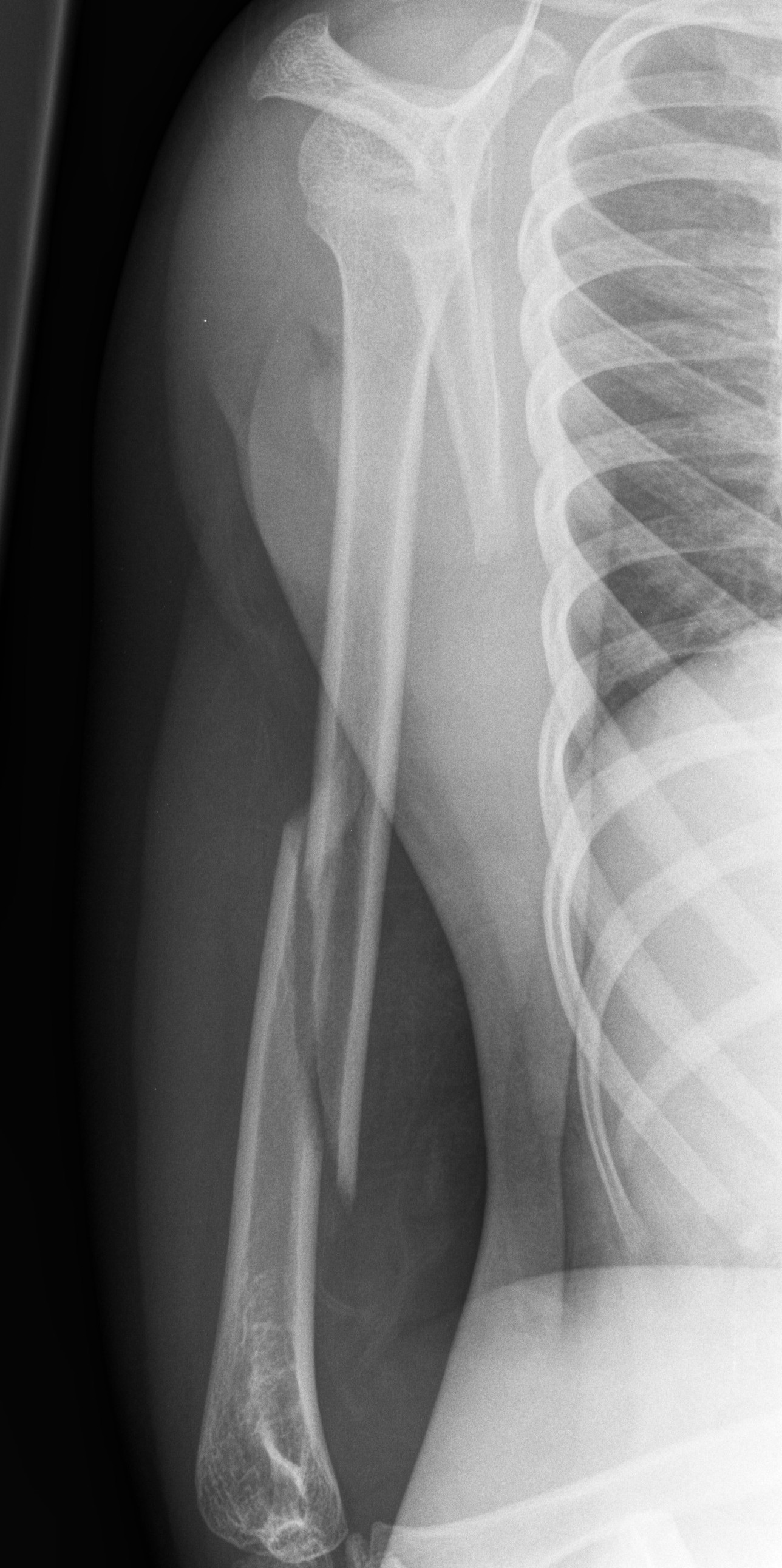
Above: Spiral fracture of shaft of humerus

Above: Completely displaced proximal humerus fracture
References
- McRae R, Max Esser M, Practical Fracture Treatment Fifth Edition, Churchill Livingstone, 2008
- Rang M, Pring ME, Wenger DR. Kluwer W, Rang's Children's Fractures Fourth edition. Wolters Kluwer, 2018
| Endorsed by: |
Co-director Surgical Services (Nursing) |
Date: |
Feb 2024 |
This document can be made available in alternative formats on request for a person with a disability.