Fractures - Elbow
Disclaimer
These guidelines have been produced to guide clinical decision making for the medical, nursing and allied health staff of Perth Children’s Hospital. They are not strict protocols, and they do not replace the judgement of a senior clinician. Clinical common-sense should be applied at all times. These clinical guidelines should never be relied on as a substitute for proper assessment with respect to the particular circumstances of each case and the needs of each patient. Clinicians should also consider the local skill level available and their local area policies before following any guideline.
Read the full CAHS clinical disclaimer.
|
See Fractures – Overview for General Assessment and Management
Mechanism of Injury
- Most common mechanism is a fall onto an outstretched hand (FOOSH) with hyperextension of the elbow.
- Direct blow or fall onto the elbow may also cause a fracture.
- Non-accidental injury is unlikely unless the child is non-ambulatory.
Examination
- There is usually swelling, tenderness and a limited range of motion of the elbow
- Obvious deformity and antecubital bruising will be seen in displaced supracondylar fractures
- Be wary of signs and symptoms of compartment syndrome if there is marked swelling of the elbow.
Imaging
- Request an elbow X-ray (true lateral and AP views are required). This should include the distal third of the humerus and proximal third of the radius and ulna.
- If concerned about a radial head fracture, an oblique view should also be done.
Elbow X-Rays in children can be difficult to interpret. A systematic approach should detect most elbow fractures.
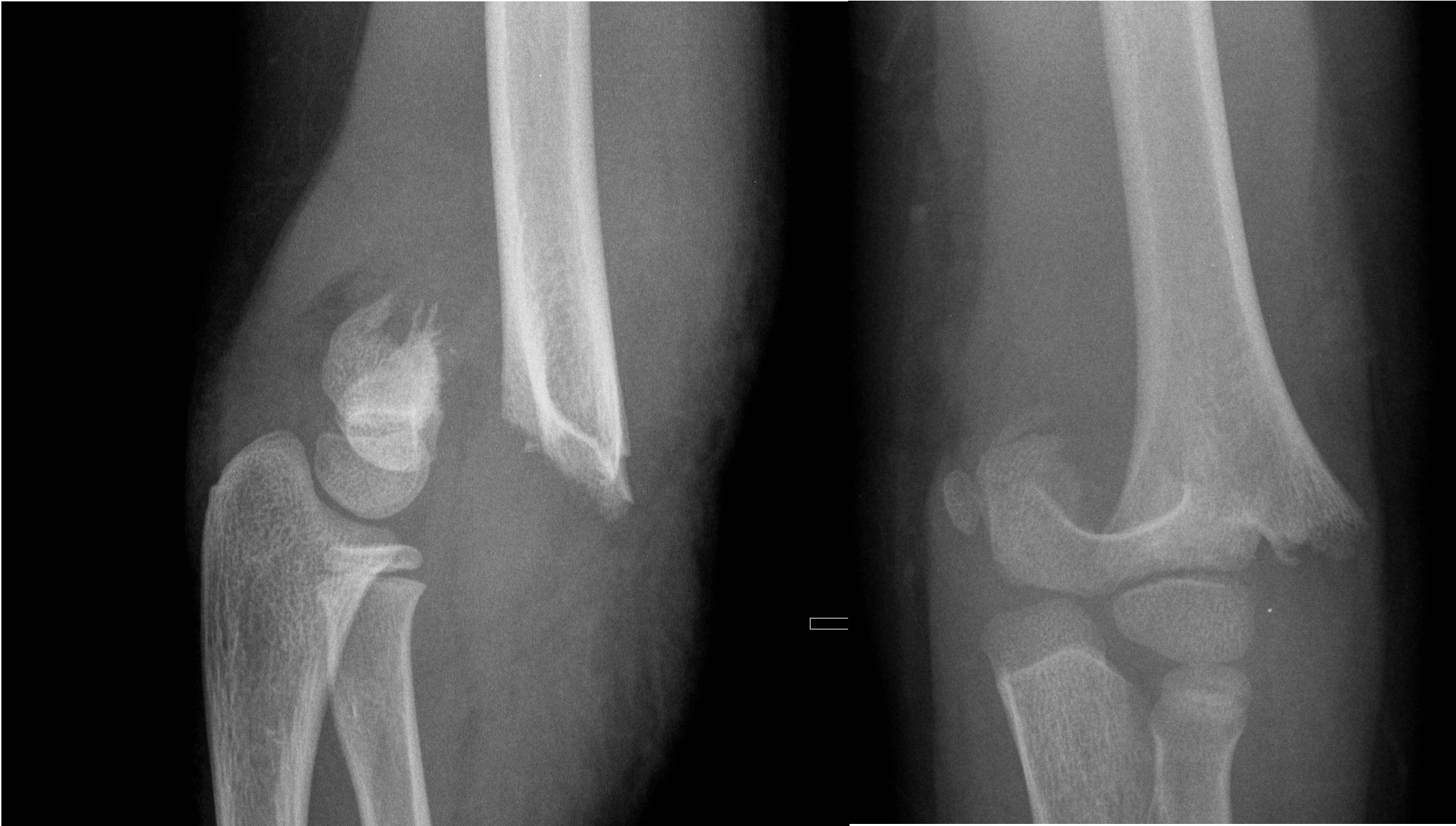
1. Ensure true lateral view of humerus
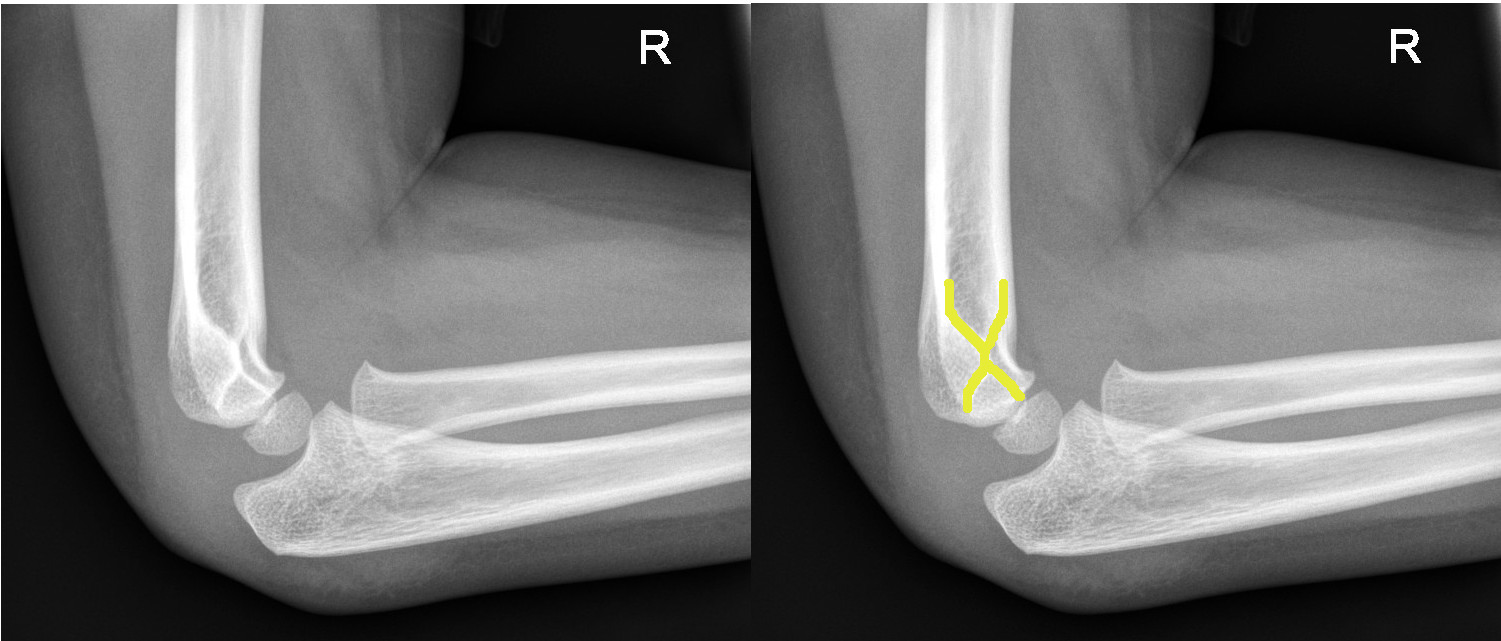
The 'Hourglass Sign' indicates a true lateral view
2. Assess the radiological lines of normal anatomy on lateral elbow X-Ray
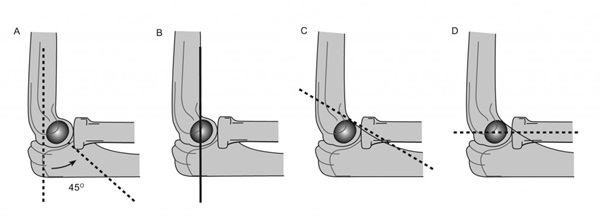
A: Normal 45 degrees anterior angulation of lateral condyle relative to humerus shaft.
B: Anterior humeral line should pass through the middle of the capitellum.
C: Coronoid line: a line extended proximally along the anterior border of the coronoid process should just touch the anterior portion of the lateral condyle.
D: Radio-capitellar line: a line drawn through the long axis of the radius should bisect the capitellum, irrespective of the degree of flexion or extension of the elbow (the X-Ray must be a true lateral view for this to apply). If the line does not pass through the capitellum, look for an associated ulnar fracture (Monteggia fracture – see Fractures - Forearm).
3. Fat pad signs
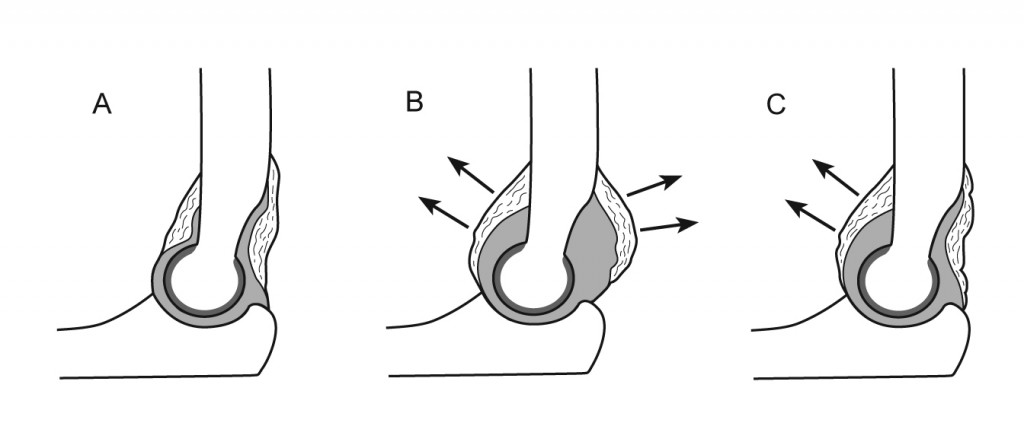
A: Normal relationship of the two elbow fat pads. Normally, the ANTERIOR fat pad may be visible as a dark triangle anterior to the distal humerus. This is only abnormal if elevated - "sail sign". Any visible POSTERIOR fat pad is abnormal.
B: Intra-articular effusion displacing both fat pads (visible as dark radiolucent areas anterior and posterior to the distal humerus).
C: Intra-articular effusion displacing only the anterior fat pad (dark radiolucent area noticeably anterior to expected position).
Example X-rays
 |
Anterior fat pad seen but NOT elevated, so NOT a joint effusion |
 |
Anterior fat pad elevated off anterior surface of humerus = joint effusion |
 |
A posterior fat pad is always abnormal |
4. Look for any cortical disruption
- Follow the anterior and posterior humerus looking for any cortical disruption.
5. Look at the contour of the radial head
- Any subtle angulation may indicate a fracture of the radial head.
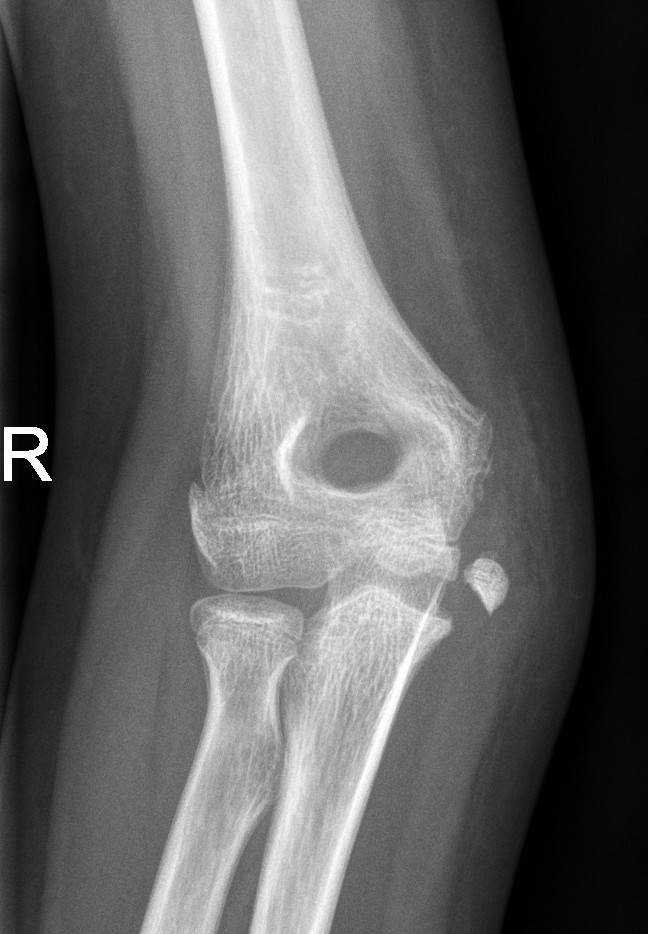
6. Look for obvious fracture lines on the AP view
 |
Supracondylar fracture evident on the AP view |
7. Assess ossification centres
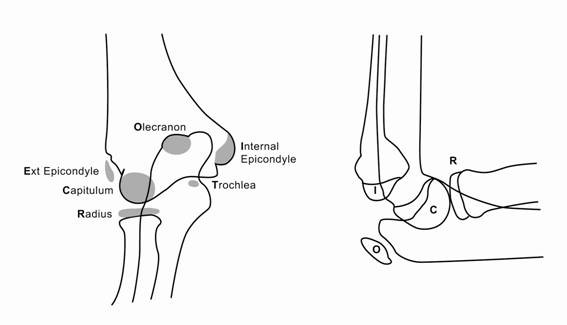
- Ensure all ossification centres present are appropriate for age.
- A lateral epicondyle fracture is commonly missed in younger children.
- Ossification centres appear in the following order (CRITOE):
- Capitellum (1 year)
- Radial head (3 years)
- Internal (Medial) epicondyle (5 years)
- Trochlea (7 years)
- Olecranon (9 years)
- External (lateral) epicondyle (11 years)
Specific management
Supracondylar fractures
Positive fat pad, but no definite fracture seen
- Treat as undisplaced supracondylar fracture (below).

Undisplaced supracondylar fracture (Gartland type 1)1
- Collar and cuff with 90 degrees flexion.
- Orthopaedic Fracture clinic follow up in 7-10 days.

Non-displaced supracondylar fracture
Displaced supracondylar fracture with an intact posterior cortex (Gartland type 2)
- Discuss with ED Consultant or Orthopaedic team regarding possible treatment
- High collar and cuff
- High collar and cuff and re-X-ray
- Admission for manipulation under anaesthetic (MUA)
- Application of a high collar and cuff uses the triceps to reduced posterior angulation of the fracture.
- Consider analgesia / sedation such as Intranasal Fentanyl and / or Nitrous Oxide / Oxygen (50:50): Self Demand – Clinical Practice Manual (internal WA Health only).
- Check radial pulse post application.

Supracondylar fracture with posterior angulation
Off-ended supracondylar fractures (Gartland Type 3)
- High risk of neurovascular compromise.
- Requires urgent Orthopaedic review and open reduction and internal fixation (ORIF) in the operating theatre.
- If applying a resting slab in ED, plaster arm in current position. Do not flex elbow.
Displaced supracondylar fracture
Medial Epicondyle Fractures
- Medial epicondyle fractures are often missed because they are mistaken as an ossification centre. Assess ulnar nerve function in any medial epicondyle fracture.
Undisplaced medial epicondyle fractures
- Above elbow plaster backslab at 90 degrees flexion with follow up in Orthopaedic Fracture clinic in 7-10 days.
Displaced medial epicondyle fractures
- Discuss with the Orthopaedic team for further management.
Displaced medial epicondyle
Lateral condyle fractures
- All lateral condyle fractures should be discussed with the Orthopaedic team for further management. They are generally unstable and prone to displacement and often require operative fixation.
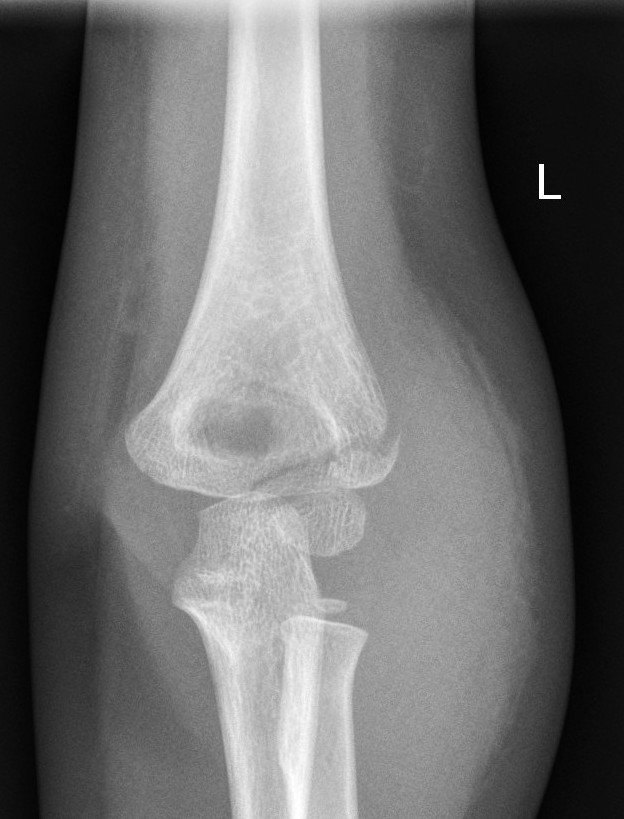
Lateral condyle fracture
Olecranon fractures
- Olecranon fractures are often seen in combination with other elbow fractures (lateral condyle, supracondylar, radial neck or radial head dislocation).
Undisplaced olecranon fractures
- Above elbow plaster backslab at 90 degrees flexion with Orthopaedic Fracture clinic follow up in 7-10 days.
Displaced olecranon fractures
- Should be discussed with the Orthopaedic team for further management.
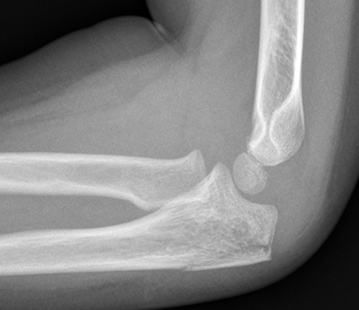
Non-displaced Olecranon fracture
Radial Head and Neck Fractures (Proximal Radius)
- Minimally displaced radial head and neck fractures with < 30 degrees angulation
- Above elbow plaster backslab at 90 degrees flexion with Orthopaedic Fracture clinic follow up in 7-10 days.
- Displaced fractures or > 30 degrees angulation
- should be discussed with the Orthopaedic team for reduction.
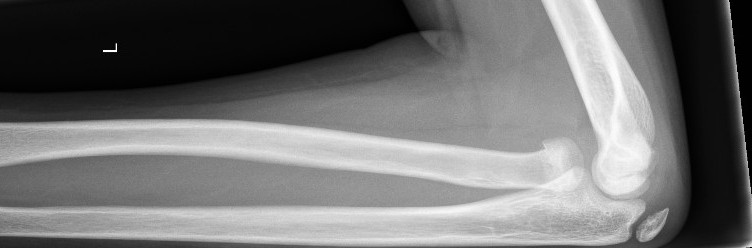
Radial neck fracture
References
- Study of treatment methods for undisplaced supracondylar humeral fractures in children. GEKO: 4016
- McRae R, Max Esser M, Practical Fracture Treatment Fifth Edition, Churchill Livingstone, 2008
- Rang M, Pring ME, Wenger DR. Kluwer W, Rang's Children's Fractures Fourth edition. Wolters Kluwer, 2018
| Endorsed by: |
Nurse Co-Director, Surgical Services |
Date: |
Mar 2024 |
This document can be made available in alternative formats on request for people with disability.