Fractures - Distal forearm or wrist
Disclaimer
These guidelines have been produced to guide clinical decision making for the medical, nursing and allied health staff of Perth Children’s Hospital. They are not strict protocols, and they do not replace the judgement of a senior clinician. Clinical common-sense should be applied at all times. These clinical guidelines should never be relied on as a substitute for proper assessment with respect to the particular circumstances of each case and the needs of each patient. Clinicians should also consider the local skill level available and their local area policies before following any guideline.
Read the CAHS clinical disclaimer.
|
See Fractures – Overview for General Assessment and Management
Mechanism of injury
The most common mechanism of injury is a fall onto an outstretched hand.
Examination
- There is usually localised tenderness and swelling with decreased range of movement.
- Limitation in supination may be a sign of minor buckle fractures.
- Clinical deformity is usually evident in displaced fractures (most commonly dorsal displacement and angulation).
- In children over 10 years of age, look for clinical signs of a scaphoid fracture: anatomical snuffbox tenderness, pain on axial compression of thumb, and pain on supination against resistance.
Imaging
- A wrist X-ray should have AP (anterior-posterior) and lateral views and include the proximal half of the metacarpals and distal third of the radius and ulna.
- A scaphoid X-ray series should have four views. Be aware the scaphoid only starts to ossify at 5 years of age.
Specific management
Buckle fractures6
- Buckle (or torus) fractures are most commonly seen in the distal radial metaphysis and are a result of compressive forces from an axial load on softer bones in children
- X-ray changes may be subtle with mild cortical bulging on the AP view and angulation on the lateral view may be evident.

Simple dorsal buckle fracture of the distal radius and ulna with minimal dorsal angulation
Simple dorsal buckle fractures must have ALL of the following features:
- No involvement of the volar surface
- Less than 15 degrees dorsal angulation
- No cortical breach
- Involves the distal third of the radius
- No greenstick or complete fracture of the ulna (buckle of the ulna is acceptable)
Management
- Manage in a wrist splint worn day and night for 3 weeks with no contact sports for a further 3 weeks after splint removal.1,2,3
- No specific follow up is needed.
- If a wrist splint is unavailable, use a below elbow plaster back slab instead.
- If a buckle fracture does NOT have all of the above features, manage as a metaphyseal fracture (see below).
Buckle fractures that should not be managed in a wrist splint
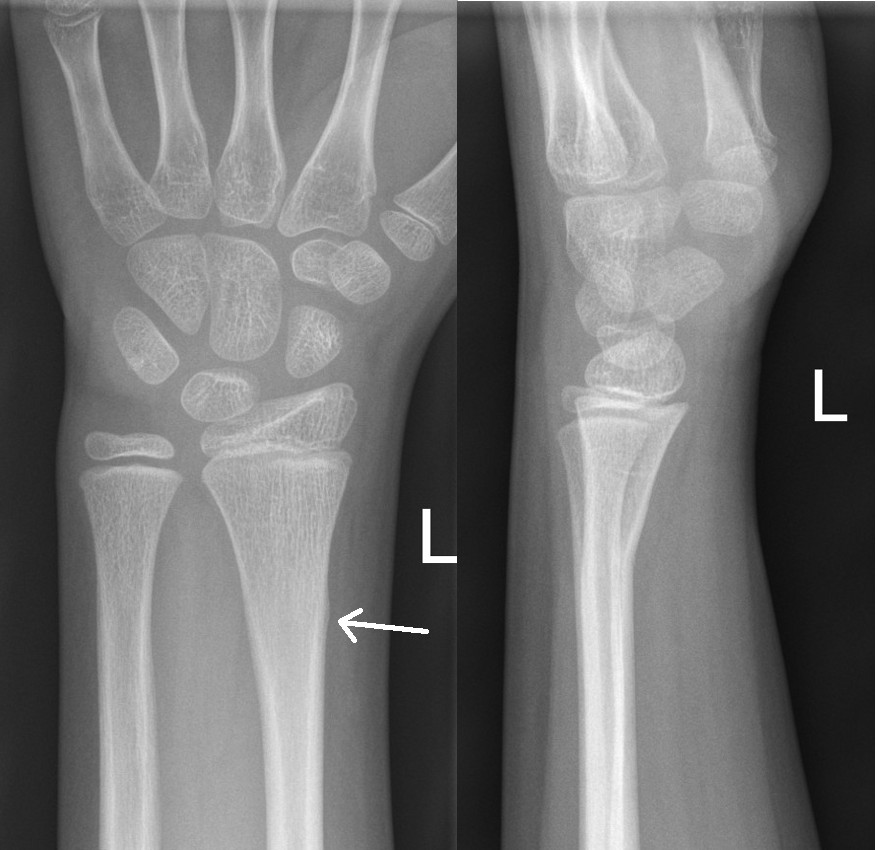
Left image: Buckle fracture with volar angulation (see arrow)
Right image: Disruption of cortex of volar aspect of radius (see arrow)
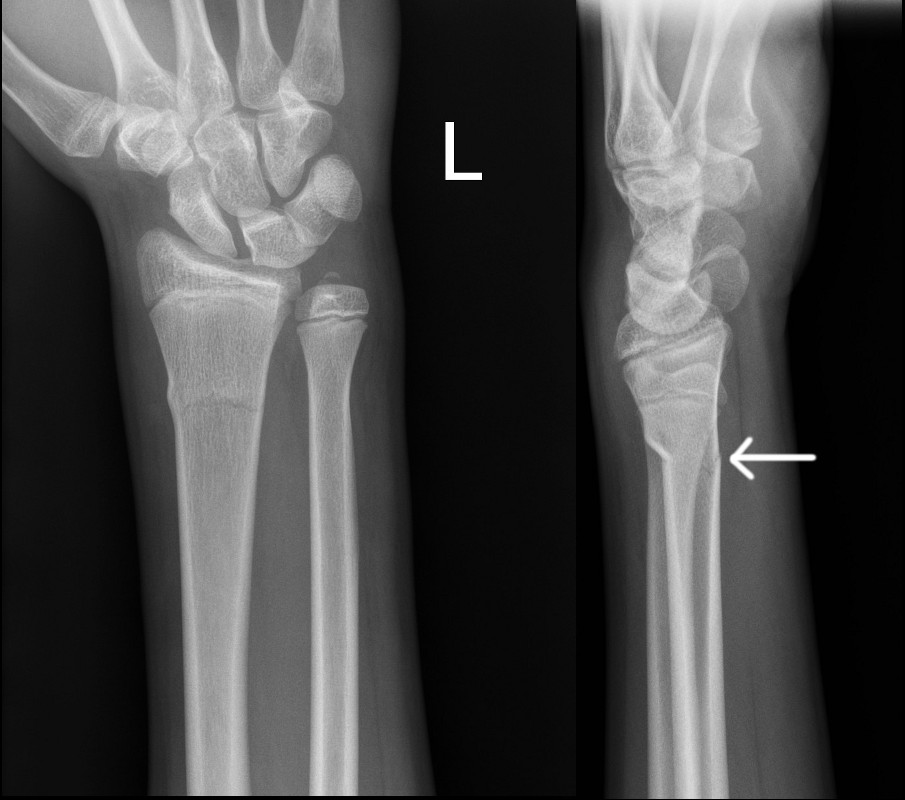
Metaphyseal Fractures
- Isolated radius fractures are acceptable, but ulna fractures are usually associated with a radius fracture or radial head dislocation.
- When both bones are involved, they often each have a different fracture type, a combination of complete, greenstick, buckle, or plastic bowing deformity.
Undisplaced distal radius fractures
- Below elbow plaster backslab with Orthopaedic Fracture clinic follow up in 7-10 days.
Undisplaced distal radius and ulna fractures
- Above elbow plaster backslab with Orthopaedic Fracture clinic follow up in 7-10 days.
Fractures with > 20° dorsal or > 10° volar angulation or clinical deformity
- Discuss with ED senior doctor or Orthopaedic team for reduction.
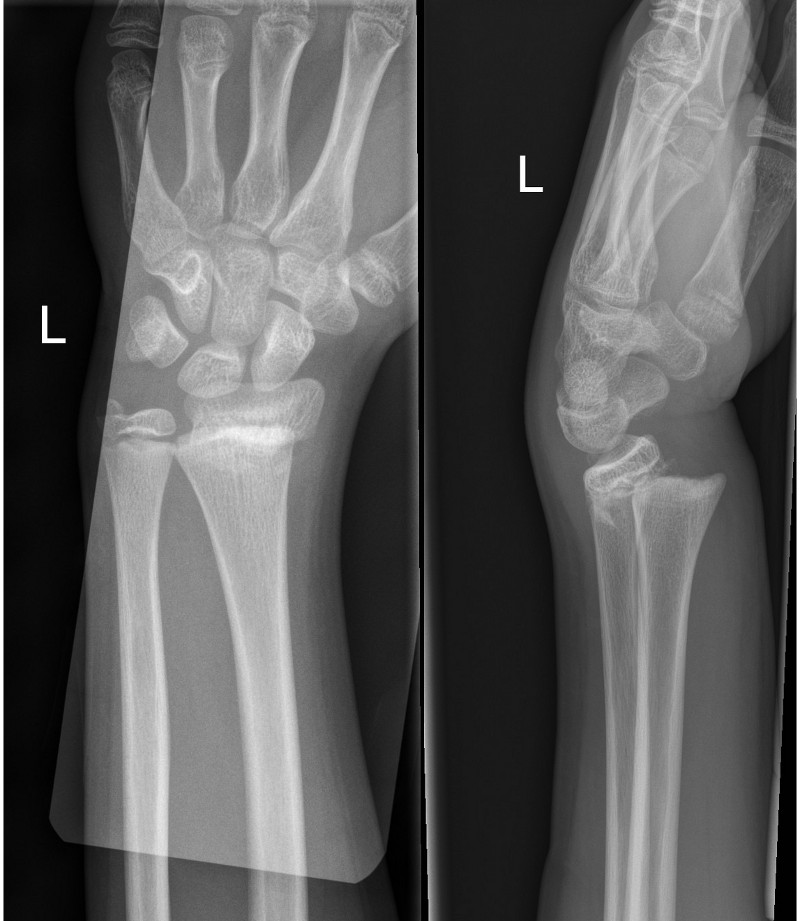
Left image: Transverse fracture of distal radius with 15 degree dorsal angulation
Right image: Completely displaced fracture of distal radius and ulna
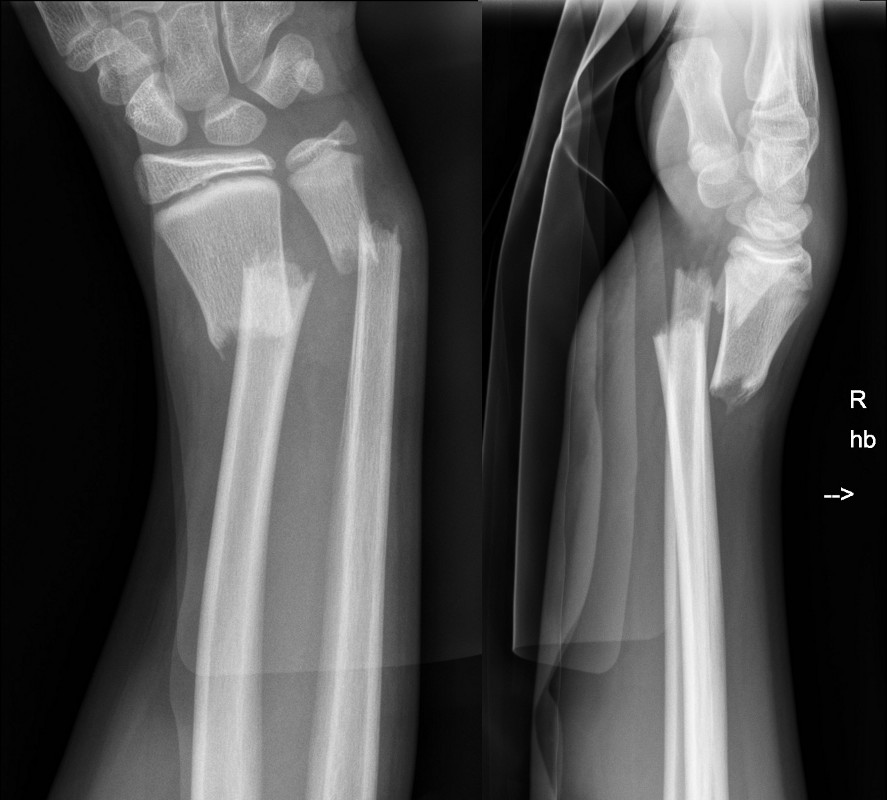
Galeazzi fracture dislocation
- A rare fracture of the distal half of the radial shaft with a disrupted distal radio-ulnar joint.
- Ensure the wrist X-ray is a true lateral.
- Refer to Orthopaedic team for reduction.

Galeazzi fracture dislocation
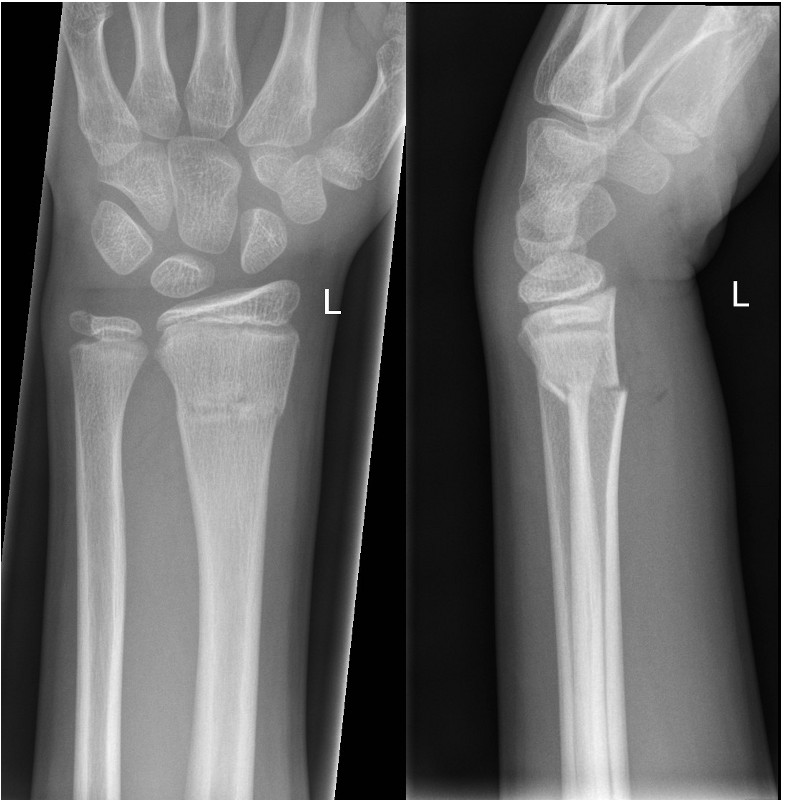
Radial physeal fractures
- Fractures involving the growth plate are usually Salter-Harris II fractures.
- Undisplaced Salter-Harris I and V fractures may not be obvious on X-Ray – immobilise in a below elbow plaster backslab with GP follow up if there is clinical suspicion (point tenderness and localised swelling of the distal radius).
Salter Harris I and II fractures
- If undisplaced with no angulation, manage in a below elbow plaster backslab with Orthopaedic Fracture clinic follow up in 7-10 days.
- If displaced or > 20 degrees angulation, discuss with ED senior doctor or Orthopaedic team for reduction.

|
|

|
|
|
Salter Harris I fracture
of distal radius
|
|
Undisplaced S-H II fracture
of distal radius
|
|
|
 |
|
|
|
|
S-H II fracture with dorsal and
radial displacement
|
|
|
|
|
Salter Harris III and IV fractures
- Refer to the Orthopaedic team.
Scaphoid fractures
- Suspect in children > 10 years old only.
- Not always evident on initial X-ray.
Displaced scaphoid fractures
- Refer to Orthopaedic team.
Undisplaced scaphoid fractures
- Below elbow plaster backslab with Orthopaedic Fracture Clinic follow up in 7-10 days.
Suspected scaphoid fracture with normal X-ray
- Wrist splint with Orthopaedic Fracture clinic follow up in 7-10 days.

A: Undisplaced distal scaphoid fracture
B: Sclerotic line in follow up X-ray 2 weeks later
Monteggia Fracture Dislocation
- Fracture of the ulna shaft with dislocation of the radial head.
- The ulna fracture is usually obvious whereas the radial head dislocation can be missed.
- Request an elbow X-ray and ensure the radial shaft is aligned with the capitellum on the lateral view.
- Refer to Orthopaedic team for reduction.

Monteggia Fracture
References
- A Randomized Controlled Trial of Removable Splinting Versus Casting for Wrist Buckle Fractures in Children. Plint A. PEDIATRICS Volume 117, Number 3, March 2006
- Common Paediatric Fractures Treated with Minimal Intervention. Boutis K. Pediatr Emer Care 2010:26
- Interventions for treating wrist fractures in children. Abraham A, Handoll HHG, Khan T, The Cochrane Library 2009, Issue 3
- Rang M, Pring ME, Wenger DR. Kluwer W, Rang's Children's Fractures Fourth edition. Wolters Kluwer, 2018
- McRae R, Max Esser M, Practical Fracture Treatment Fifth Edition, Churchill Livingstone, 2008
- Rowlands et al. Putting evidence based protocols into practice- a paediatric buckle fracture pathway. Arch Dis Childh. 2012;97(1):A141-A142
| Endorsed by: |
Co-director Surgical Services (Nursing) |
Date: |
Mar 2024 |
This document can be made available in alternative formats on request for a person with a disability.