Trauma - Serious injury
Disclaimer
These guidelines have been produced to guide clinical decision making for the medical, nursing and allied health staff of Perth Children’s Hospital. They are not strict protocols, and they do not replace the judgement of a senior clinician. Clinical common-sense should be applied at all times. These clinical guidelines should never be relied on as a substitute for proper assessment with respect to the particular circumstances of each case and the needs of each patient. Clinicians should also consider the local skill level available and their local area policies before following any guideline.
Read the full CAHS Emergency Department disclaimer
|
Aim
To guide PCH ED staff with the assessment and management of serious injury.
This guideline gives an overview of the approach to the seriously injured child including the primary and secondary survey.
Background1,2
- Trauma/serious injury is a leading cause of death in children in Australia
- Early ABCDE (Airway, Breathing, Circulation, Disability, Environment) interventions improve morbidity and mortality secondary to major trauma
- A trauma team approach should be used to manage seriously injured children
Key points
- The main causes of serious injury in children are due to motor vehicle accidents and falls.
- Injury prevention is the biggest factor in reducing trauma mortality but unfortunately children still continue to be injured.
- Consider NAI in cases of unexplained injury or pattern suspicious of physical assault
- All injury presentations in children under 2 years must have an Early Childhood Injury Proforma (MR301.3) completed. (internal WA Health only)
- Primary assessment and early ABCDE interventions will avoid some deaths and prevent late complications in children involved in major trauma.
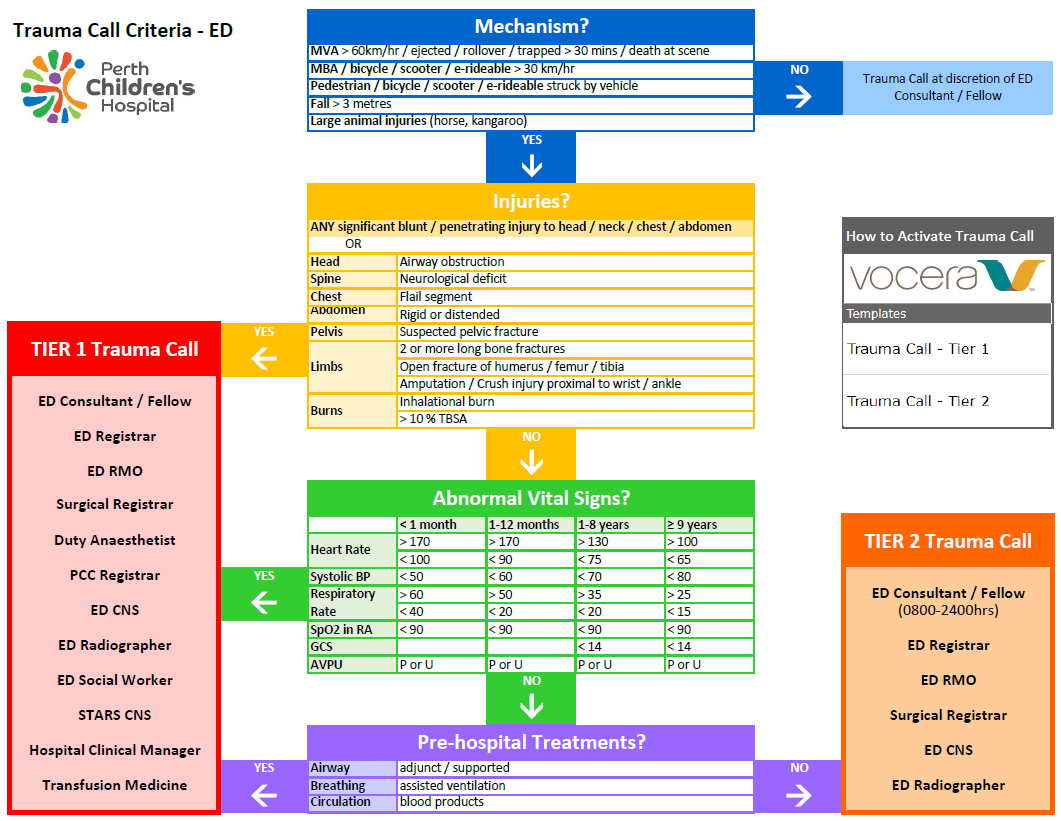
- At PCH, a two tiered trauma call system is used based on mechanism, injuries, vital signs, and treatment (see below). The trauma team will consist of staff from the Emergency Department and Paediatric Surgery, with Paediatric Critical Care Unit (PCC), and anaesthetic teams attending for Tier 1 trauma calls.
- This multidisciplinary trauma team will follow a structured approach to manage seriously injured patients.
- This structured approach initially focuses on identifying and treating immediate threats to life – the primary survey.
- Following the initial primary survey and resuscitation, the structured approach is again used for a secondary survey to identify other key injuries which require emergency treatment to stabilise the patient and prevent secondary insult.
- It is recommended that all healthcare workers who work with injured children undertake an Advanced Paediatric Life Support (APLS), Emergency Management of Severe Trauma (EMST) course or similar to provide the skills needed to assess and manage seriously injured children.
Preparation1,2,3
- History pre-arrival
- Obtain information from the trauma alert phone call – use ATMISTER acronym
- A = Age / sex
- T = Time of incident
- M = Mechanism of injury
- I = Injury suspected
- S = Signs including vital signs, Glascow Coma Scale (GCS)
- T = Treatment so far
- E = Estimated time of arrival to PCH ED
- R = Requirements e.g. blood, specialist services
- Allocate roles
- Primary survey doctor, airway / breathing doctor and nurse, circulation doctor and nurse, scribe, team leader, medications nurses and family support.
- Activate a Trauma Call - Tier 1 or Tier 2 for all major trauma patients presenting to PCH ED: Trauma Call Criteria - ED below.
- For direct inter-hospital trauma transfers to PCC: refer to Trauma Call Criteria - PCC.
History on Arrival
- Unless there is a life-threatening injury, then on arrival a succinct ‘hands off’ handover should occur
- A detailed history of the incident should be sought including:
- Mechanism of injury
- Time of injury
- Other fatalities
- Obvious injuries
- Observations
- Pre-hospital treatment
- Any known past medical history and allergies
Assessment1,2,3
- A structured, systematic approach is essential when assessing seriously injured children
- Primary survey using an ABCDE approach is a simple and highly effective method in major trauma.
- Assume cervical spine injury in all trauma patients
- Treat problems immediately as thay are found during the primary survey, before moving on.
Primary survey
- The primary survey involves a rapid structured assessment of catastrophic external haemorrhage, Airway, Breathing, Circulation, Disability and Exposure.
- Treat life threatening issues immediately as they are discovered during the primary survey before moving on.
Assessment
- Look for open wounds with active bleeding
- Look for blood pooling on the sheets / floor
|
Management
- Apply direct pressure and / or a tourniquet above the wound
- Give tranexamic acid 15 mg/kg (maximum 1000 mg) IV1
|
Assume cervical spine injury in any major trauma patient
Immobilise cervical spine |
Assess airway patency and signs of obstruction:
- Stridor
- Stertor
- Hoarse voice
- Bruising and swelling
|
Resuscitation
- Suction if necessary
- Jaw thrust (head tilt is contraindicated if there is suspicion of cervical spine injury)
- Oropharyngeal airway (nasopharyngeal airway contraindicated if there is suspicion of a base of skull fracture)
- Endotracheal intubation
- Surgical airway
|
Fully expose the neck and chest
Look, listen and feel
Provide oxygen via a non-rebreather mask with a reservoir
|
Assess
- Bruising, wounds
- Symmetry of chest expansion
- Trachea - midline?
- Respiratory rate
- Respiratory effort - nasal flare, recession, accessory muscle use
- Air entry
- Oxygen saturation
- Percussion note
- Effects - heart rate, skin colour, mental state
|
Urgently exclude and treat
- Airway obstruction
- Tension pneumothorax
- Open pneumothorax
- 3 way occlusive dressing (while preparing for drain)
- Massive haemothorax
- Flail chest
Support ventilation as needed
- Bag valve mask ventilation
- Intubation and positive pressure ventilation
- Consider an orogastric tube (nasogastric contraindicated if there is a suspicion of a base of skull fracture)
|
Assess
- Skin colour
- Heart rate
- Pulse pressure
- Mental state
- Signs of shock
- Distended neck veins
- Muffled heart sounds
- Peripheral pulses in all limbs
Examines sites of possible internal haemorrhage (chest, abdomen, pelvis, femurs, scalp)
|
Exclude and treat
Resuscitation
- Two large bore cannulas (take blood for full blood count and cross match)
- Fluid resuscitation –
- 10-20mL/kg of sodium chloride 0.9% and repeat if necessary
- Early use of blood
- Tranexamic acid 15 mg/kg (maximum 1000 mg) IV1
- Activation of critical bleeding protocol
- Surgical intervention to stop internal bleeding (chest, abdomen, pelvis)
|
Hypoxia and shock can cause a decrease in conscious level
Any ABC problem is to be addressed before assuming a primary neurological problem |
Assess level of consciousness, pupils, posture and blood glucose.
- Conscious level - Alert Voice Pain Unresponsive (AVPU) scale
- Pupil size, symmetry and reactivity
- Abnormal posturing (decorticate, decerebrate)
- Seizure activity
- Bedside glucometer reading
|
Resuscitation
|
Fully expose child and assess temperature and signs of injury
- Check core temperature
- Don't forget to log roll and check back for injuries
|
- Prevent hypothermia
- Reduce exposure during examination
- Use warmed fluids or blood products
|
Investigations
- Take blood for full blood count, urea, electrolytes and creatinine, liver function test, lipase, coagulation profile, venous blood gas and Group & Hold or Cross Match. Also test beta human chorionic gonadotrophin (beta hCG) in adolescent females.
- Consider trauma series X-rays – cervical spine, chest, pelvis
- If concerns regarding abdomen or pelvis - request a Computerised Tomography (CT) scan
- Perform a CT neck scan rather than an X-ray if already doing a CT head scan
- Other adjuncts to the primary survey include FAST scan (Focused Assessment with Sonography for Trauma), orogastric tube and bladder catheterisation.
Management
Further management
Secondary survey
- A secondary survey is performed after treating any life-threatening conditions detected during the primary survey.
- The secondary survey should be abandoned to repeat the primary survey if there is any deterioration in the patient’s condition.
- The secondary survey involves a head to toe and front to back examination to detect any non-life-threatening injuries which require further management.
- Further investigations and management will be determined by injuries found on secondary survey, e.g. specific limb X-rays, CT scans etc.
Medications
Admission criteria
- All major trauma should be admitted under the general surgical team (which at PCH is the Trauma Team).
- Other surgical subspecialty involvement will be determined by the injuries sustained.
Management paperwork
- All major trauma patients should have documentation done on an ED Trauma Sheet (MR 301.04). These are A3 folded forms, located in the Resuscitation Bay and Doctor’s offices.
References
- Advanced Paediatric Life Support: The Practical Approach. 6th edition Australia and New Zealand Version. Wiley-Blackwell, 2016.
- Fleisher and Ludwig's Textbook of Pediatric Emergency Medicine Eighth Edition. Journal of Pediatric Critical Care 8.2 (2021): 116. Web. Kundan Mittal.
- Textbook of Paediatric Emergency Medicine 3rd Edition Cameron P, Browne GJ, Mitra B, et al (2018) Publisher: Elsevier Edition
- AMH Children’s Dosing Companion January 2022; Cited 5 May 2022; Mannitol - AMH Children's Dosing Companion (health.wa.gov.au) Mannitol - AMH Children's Dosing Companion (health.wa.gov.au)
| Endorsed by: |
CAHS DTC |
Date: |
Apr 2025 |
This document can be made available in alternative formats on request for a person with a disability.